Cardiac Function
Introduction to Cardiac Function
Learning Objectives
- Explain the excitation-contraction coupling in the cardiac myocyte.
- Describe how the autonomic nervous system modulates heart rate and force of contraction.
- Explain Frank-Starling mechanism with the length-tension relationship.
Excitation-Contraction Coupling in Cardiac Myocytes
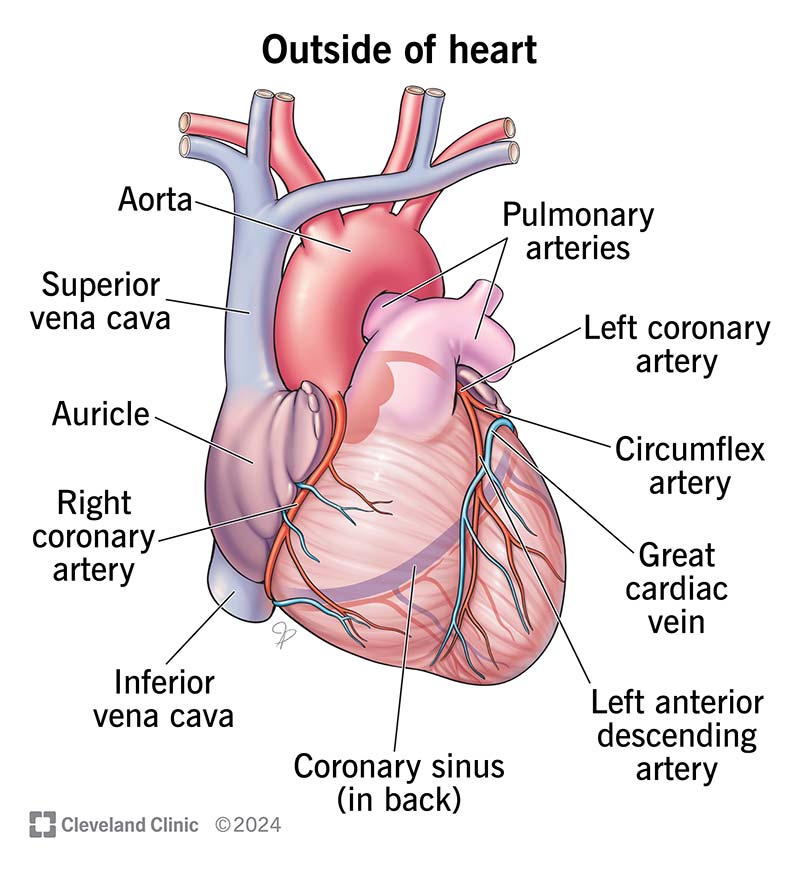
Excitation-contraction coupling starts with an action potential, which travels along the sarcolemma and down the T-tubules, leading to depolarization. This depolarization triggers the opening of voltage-gated calcium channels, allowing calcium ions to enter the cell from the extracellular space.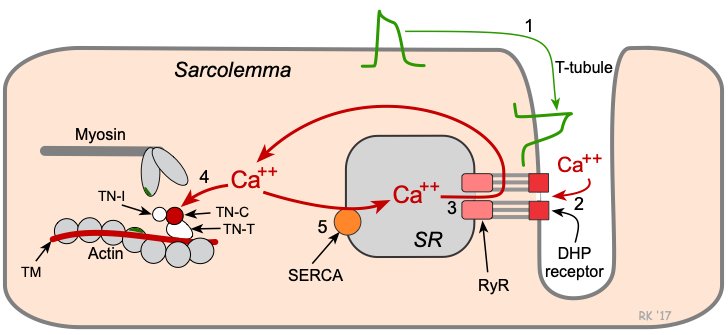
The influx of calcium through these channels then stimulates the release of additional calcium from the sarcoplasmic reticulum (SR) through ryanodine receptors in a process known as calcium-induced calcium release (CICR). This sudden increase in intracellular calcium concentration allows calcium to bind to the troponin-C component of the troponin complex on the thin filaments, leading to a conformational change that moves tropomyosin away from actin-binding sites. This exposure allows the actin-myosin interaction, leading to cross-bridge formation and cycling, which generates force and, ultimately, contraction.

Cardiac myocyte relaxation (diastole) occurs when calcium ions are re-sequestered back into the SR by the sarcoplasmic/endoplasmic reticulum calcium ATPase (SERCA) pumps and extruded from the cell via the sodium-calcium exchanger (NCX) and plasma membrane Ca-ATPase (PMCA). The decrease in intracellular calcium concentration results in the dissociation of calcium from troponin, allowing tropomyosin to cover actin-binding sites and, thus, muscle relaxation.
Modulation of Heart Rate and Force of Contraction by the Autonomic Nervous System
The autonomic nervous system (ANS) exerts significant control over the heart rate (chronotropy) and the force of contraction (inotropy). The sympathetic and parasympathetic branches of the ANS play opposing roles in this regulation.

Sympathetic Nervous System
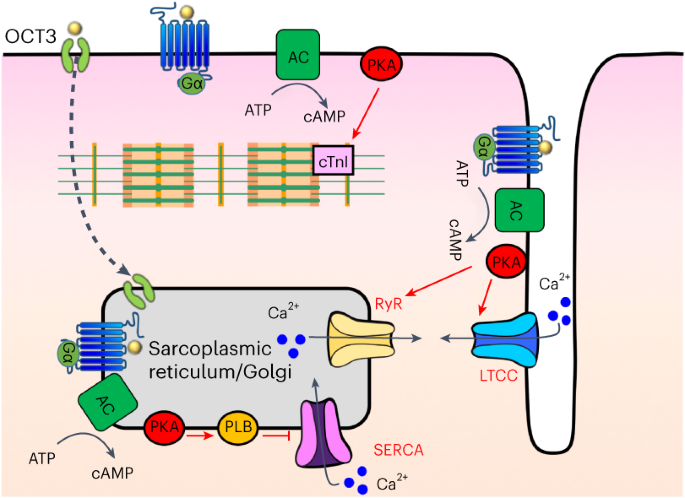
Heart Rate (Chronotropy): Sympathetic stimulation increases heart rate by releasing norepinephrine, which binds to beta-adrenergic receptors (specifically beta-1 receptors) on the pacemaker cells in the sinoatrial (SA) node. This binding activates the G-protein-coupled stimulatory pathway, increasing cyclic AMP (cAMP) production and subsequently enhancing the activity of the funny current (If) and calcium channels (ICaL), which accelerates depolarization and increases heart rate.
Force of Contraction (Inotropy): Sympathetic stimulation also enhances the force of contraction through beta-adrenergic receptor-mediated pathways that increase intracellular calcium availability. This is achieved by increasing calcium influx via L-type calcium channels and enhancing calcium release from the SR, thereby increasing cross-bridge cycling and force generation.
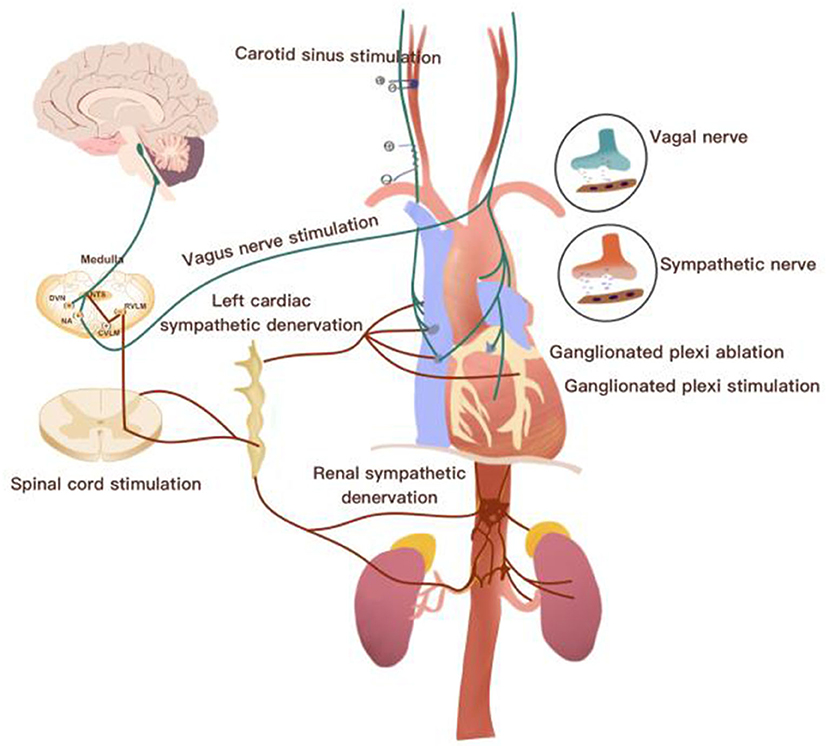
Parasympathetic Nervous System
Heart Rate (Chronotropy): Parasympathetic stimulation decreases heart rate via the release of acetylcholine, which binds to muscarinic receptors (M2) on pacemaker cells. This activation causes the opening of potassium channels (I_KACh), leading to hyperpolarization and a reduction in the cardiac pacemaker potential. This slows down the depolarization rate and decreases heart rate.
Force of Contraction (Inotropy): While the parasympathetic influence on the force of contraction is less pronounced in ventricles, it can still exert a negative inotropic effect on the atria by decreasing calcium influx and reducing the gradient for calcium-induced calcium release.

Frank-Starling Mechanism and Length-Tension Relationship
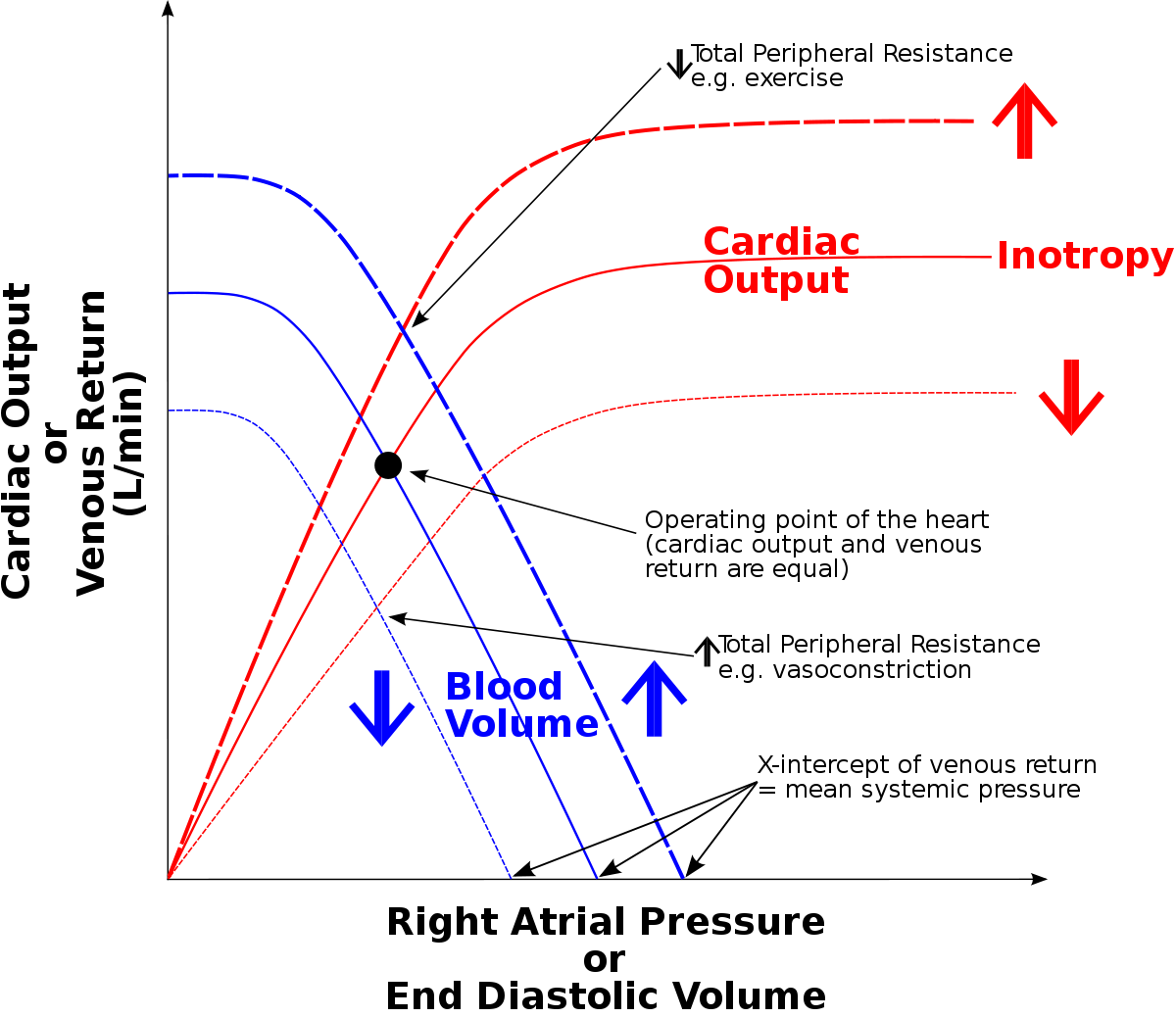
The Frank-Starling mechanism describes the relationship between the length of myocardial fibers (preload) and the force of contraction during systole. This principle states that an increase in the end-diastolic volume (EDV) stretches the myocardial fibers, which leads to a more forceful contraction.
Length-Tension Relationship
Resting Length: At resting length, sarcomeres have optimal overlap between actin and myosin filaments, enabling maximal cross-bridge formation during contraction.
Increased Preload: When the preload is increased, it stretches the sarcomeres beyond their resting length, increasing the potential for cross-bridge formation. However, if the fibers are stretched too much, the overlap between actin and myosin decreases, reducing force production.
Increased Force of Contraction: The initial increase in sarcomere length stretches the heart muscle, leading to increased troponin sensitivity to calcium, enhanced calcium binding, and ultimately greater force of contraction. This relationship highlights the heart's intrinsic ability to adjust its pumping capacity in response to changes in venous return.

Understanding these mechanisms is critical to appreciate how the heart operates efficiently under varying physiological conditions and how pathophysiological changes can impact cardiac function.
Here's a fun little AI-generated song: