CV Effects of the Autonomic Nervous System (ANS)
CV Effects of the Autonomic Nervous System (ANS)
Lecture Objectives
- Describe cardiovascular (CV) effects, therapeutic uses, and side effects of prototype adrenergic blockers (antagonists)
- Explain how agonist effects are modified when pretreated with blockers
- Predict blood pressure and heart rate changes when given sympathomimetics alone and in combination with ANS blockers
1. Cardiovascular Effects, Therapeutic Uses, and Side Effects of Adrenergic Blockers
Alpha-Blockers:
- Effects: Vasodilation, decreased blood pressure.
- Uses: Hypertension, BPH.
- Side Effects: Orthostatic hypotension, reflex tachycardia.
Beta-Blockers:
- Effects: Decreased heart rate, reduced cardiac output.
- Uses: Hypertension, angina, heart failure, arrhythmias.
- Side Effects: Bradycardia, fatigue, bronchoconstriction.
2. Modification of Agonist Effects with Blockers
- Alpha-Blockers: Prevent vasoconstriction by alpha-agonists; may cause "epinephrine reversal" (decreased BP).
- Beta-Blockers: Reduce heart rate and contractility effects of beta-agonists; can lead to unopposed vasoconstriction by alpha-agonists.
3. Predicting Blood Pressure and Heart Rate Changes
Sympathomimetics Alone:
- Epinephrine: Increases heart rate and BP.
- Norepinephrine: Increases BP, slight decrease in heart rate (reflex).
Combination with Blockers:
- Alpha-Blocker + Epinephrine: Decreased BP (epinephrine reversal), increased heart rate.
- Beta-Blocker + Epinephrine: Decreased heart rate, minimal effect on BP; unopposed vasoconstriction.
Cardinal Rule of Pharmacology
- Blockers are designed to block. They will inhibit underlying activation and future endogenous or exogenous stimulation.
- There will be no effect when there is nothing to block.
Agonists and Antagonists
- Agonists: Drugs that occupy receptors and activate them. Example: Achieving full activation.
- Antagonists: Drugs that occupy receptors but do not activate them. They block receptor activation by agonists, resulting in no activation. Example: Achieving no activation.

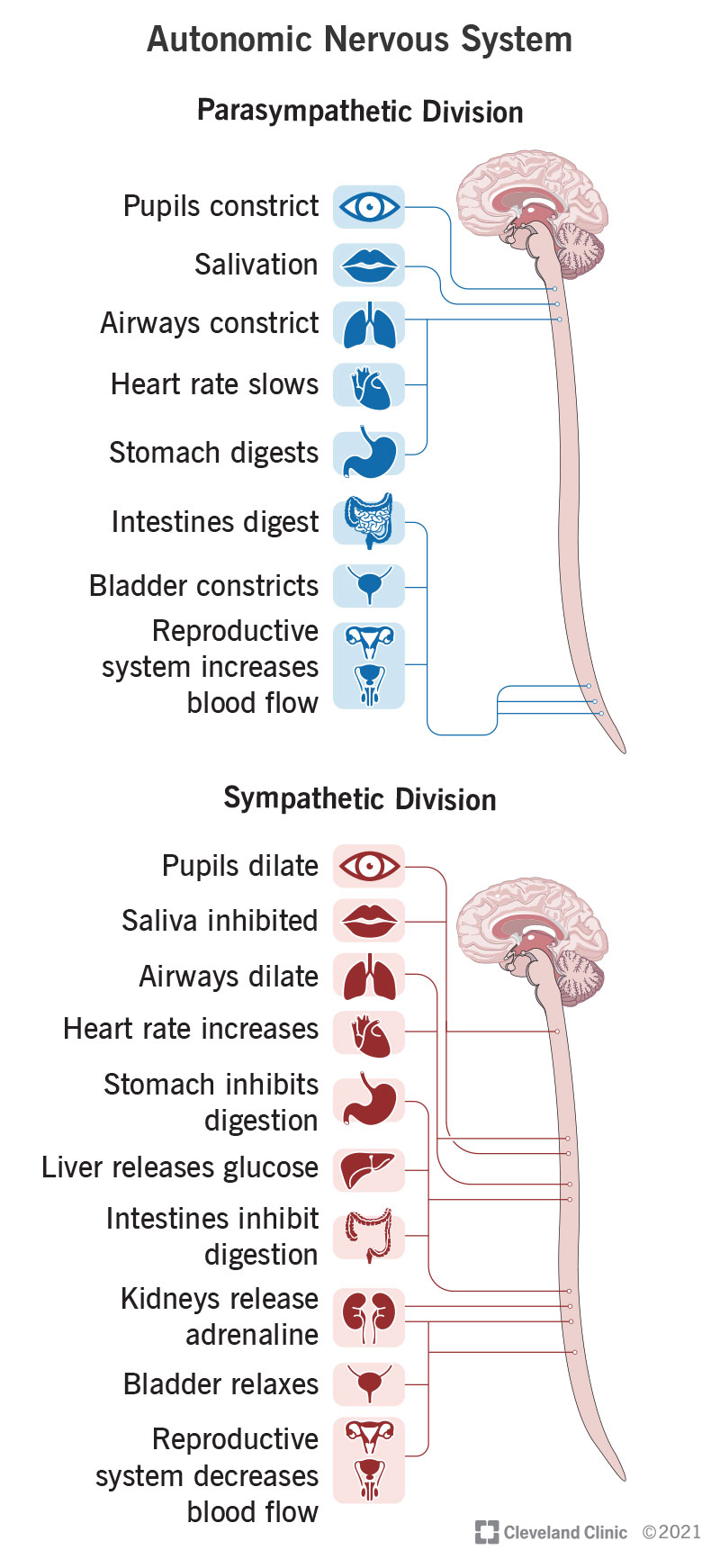
Alpha and Beta Blockers
- Alpha blockers (Xα) and Beta blockers (Xβ):
- α1: Causes vasoconstriction
- β1: Causes heart stimulation
- Vasodilation: Result of alpha blockage
- Heart suppression: Result of beta blockage
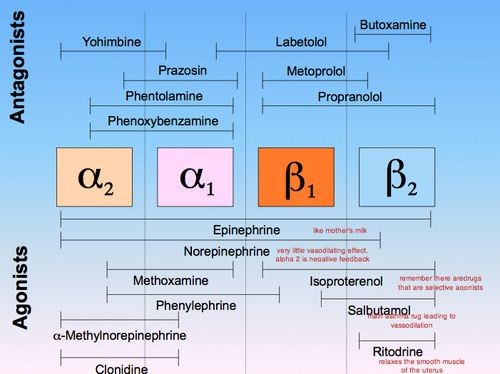
Examples of Alpha Blockers
- Phentolamine
- Phenoxybenzamine
- Prazosin (α1)

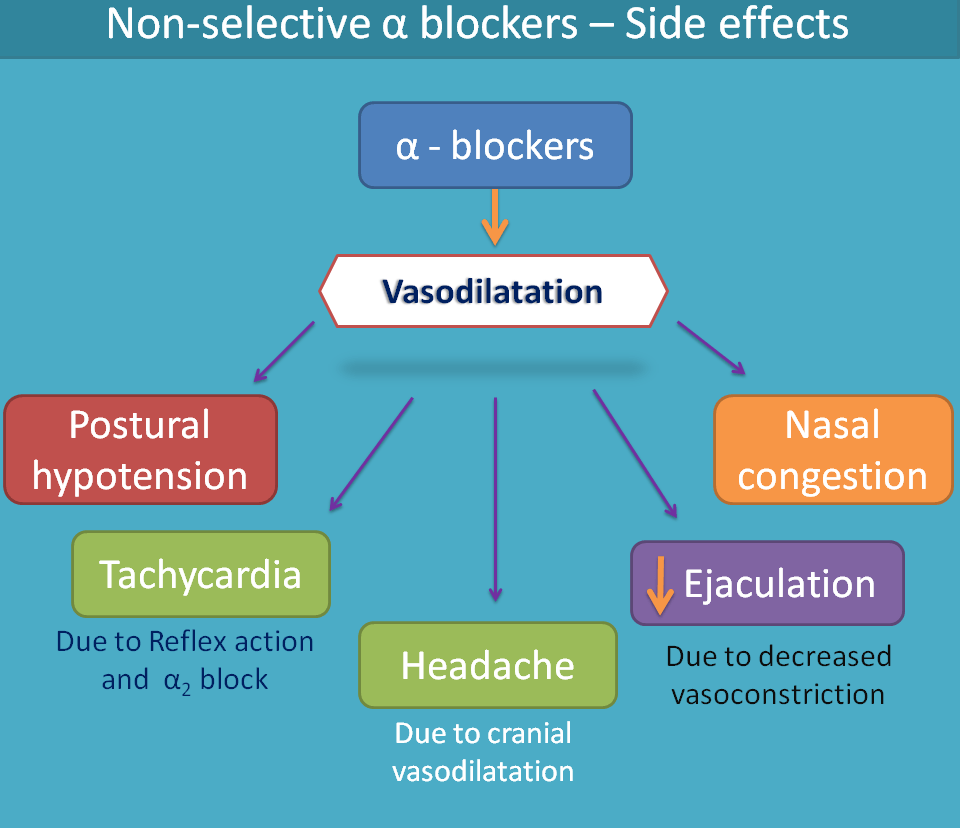
Alpha Blocker Summary
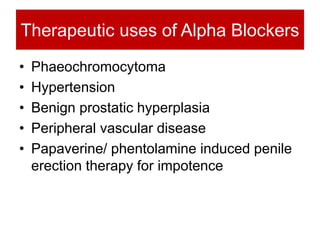
- Vasodilation and decreased blood pressure: Used in hypertensive crisis (pheochromocytoma, cocaine overdose, MAOI hypertensive crisis)
- Smooth muscle dilation: Prazosin is used for benign prostatic hyperplasia (BPH)
- Main side effects:
- Reflex tachycardia
- Orthostatic hypotension
Clinical Uses and Side Effects of Alpha Blockers
- Pheochromocytoma: Tumor in adrenal gland producing too much NE, Epi. Use phenoxybenzamine to reduce peripheral vascular resistance (PVR) and blood pressure before adding beta-blocker until surgery.
- Hypertensive crisis caused by MAOI+tyramine or cocaine: Use phentolamine to reverse vasoconstriction, but be cautious of reflex tachycardia.
- Raynaud’s disease: Abnormal vasoconstriction to extremities in response to cold/stress.
- Benign prostatic hyperplasia (BPH): Use α1-selective blockers like prazosin. Prefer once-daily α1 blockers over prazosin, which may be needed 2-4 times daily.
Reflex Tachycardia and Orthostatic Hypotension
- Reflex Tachycardia: Increase in heart rate due to baroreflex in response to low blood pressure after vasodilation.
- Orthostatic Hypotension: Drop in blood pressure when standing up, leading to potential dizziness or fainting.
Epinephrine Reversal
- Before alpha blockade: Large doses of epinephrine (Epi) act on α1, α2, β1, and β2 receptors, causing vasoconstriction (dominant α1 effect) and an increase in systemic vascular resistance (SVR) and blood pressure (BP).
- After alpha blockade: Large doses of Epi primarily act on β1 and β2 receptors due to blocked α receptors, resulting in vasodilation (β2 effect) and a decrease in SVR and BP, known as epinephrine reversal.

Beta Blockers
- Examples:
- Non-selective (β1 and β2): Propranolol, Timolol
- Cardioselective (β1): Atenolol, Metoprolol

Beta Blocker Summary
- Therapeutic Uses:
- Treat cardiac conditions (β1 block), hypertension, and glaucoma (decrease aqueous humor production with Timolol).
- Side Effects:
- β2 blockade: Bronchoconstriction and hypoglycemia.
- General side effects: Tiredness, insomnia, depression, etc.
Rationale for Beta Blocker Use in Heart Conditions
- Angina: Decrease O2 demand by reducing heart rate (HR) and contractility.
- Heart Failure: Prevent overworking; decrease mortality with specific beta-blockers like bisoprolol, carvedilol, and metoprolol.
- Arrhythmia: Slow down abnormal heart rhythm via SA or AV node modulation.
- Hypertension: This is not first-line therapy anymore, but it is useful in combination, particularly for addressing reflex tachycardia.

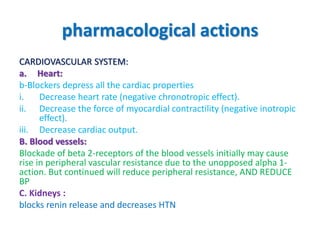
Pharmacological Actions of Beta Blockers
- Decrease HR, contractility, cardiac output (CO), and AV conduction velocity.
- It may decrease total coronary blood flow (β2 blockade) and increase airway resistance.
- In insulin-dependent diabetics, β1 antagonists are preferred to avoid hypoglycemic issues.
- Associated with increased plasma triglycerides (VLDL) and decreased HDL.
Clinical Uses of Beta Blockers
- Widespread Uses: Arrhythmia, angina pectoris, hypertension, myocardial infarction.
- Secondary Uses: Hyperthyroidism, glaucoma, migraine prophylaxis, acute dissecting aortic aneurysm, and pheochromocytoma (only after α-blockers).

Adverse Effects of Beta Blockers
- Decreased HR and CO can be problematic in congestive heart failure or bradycardia.
- Bronchoconstriction is a concern for patients with obstructive airway disease.
- Hypoglycemia risk for insulin-dependent diabetics.
- Tiredness, insomnia, depression, nightmares.
- Gastrointestinal issues: Diarrhea, heartburn.
- Skin issues: Rash and fever.
