Anticoagulant, Antiplatelet, and Fibrinolytic Therapies
Anticoagulant, Antiplatelet, and Fibrinolytic Therapies
Objectives
- Explain the pathophysiology of thrombosis underlying the acute coronary syndrome (ACS)
- Describe the targets and mechanisms of anti-coagulation therapy in ACS
- Describe the targets and mechanisms of anti-platelet therapy in ACS
- Describe the targets and mechanisms of fibrinolytic therapy in ACS
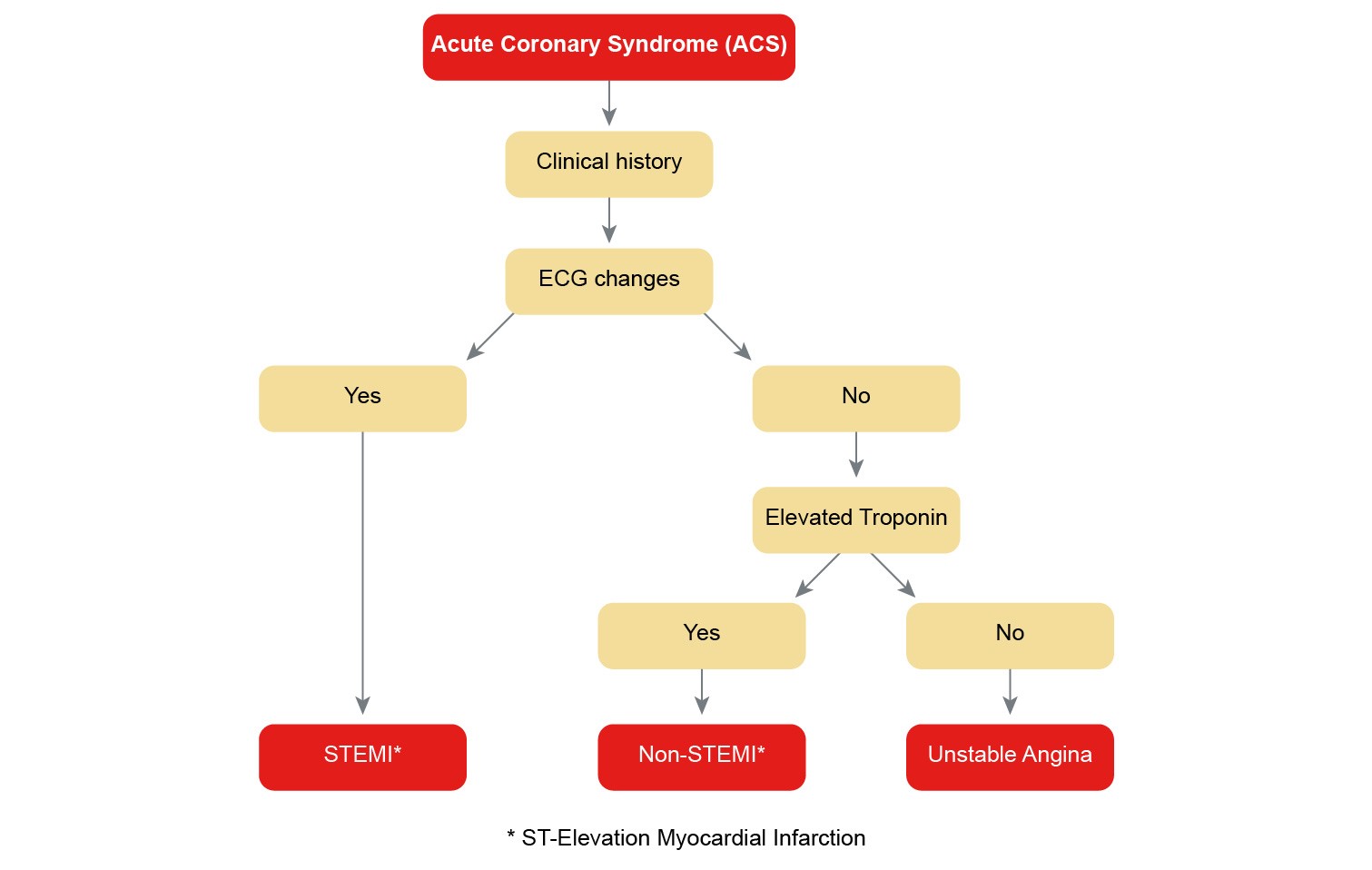
Acute Coronary Syndrome (ACS)
Acute Coronary Syndrome is an umbrella term for situations where the blood supply to the heart muscle is suddenly blocked. The primary elements involved include a "vulnerable plaque" and the occluding "thrombus."
Mechanisms of Thrombus Formation
Activation of Coagulation and Platelets
Components of the hemostatic system comprise:
- Coagulation: This involves plasma/biochemical reactions where zymogens, co-factors, and enzymes play pivotal roles.
- Platelet Response: A cellular response which leads to hemostasis under normal physiology or thrombosis in pathological states.
Thrombin is central to coagulation and ensures that enzymatic reactions remain robust. Here’s the propagation steps:
- Initiation: This involves Tissue Factor (TF) or thromboplastin
- Propagation: Various coagulation factors are activated via enzymatic reactions.
Key Players in Coagulation
- Vitamin K Epoxide Reductase Inhibitors: Warfarin (Coumadin) inhibits vitamin K dependent carboxylation of glutamate residues in coagulation factors.
- Antithrombin Dependent Inhibitors: Heparinoids like unfractionated heparin (UFH) and low molecular weight heparin (LMWH) function by activating antithrombin.
- Direct Xa Inhibitors: Such as Rivaroxaban and Apixaban, which directly inhibit factor Xa.
- Direct Thrombin Inhibitors: For instance, Argatroban and Bivalirudin.
Clinical Case Examples
- A 79-year-old man prescribed an anticoagulant requiring regular INR monitoring, most likely given a drug that inhibits vitamin K epoxide reductase (Warfarin).
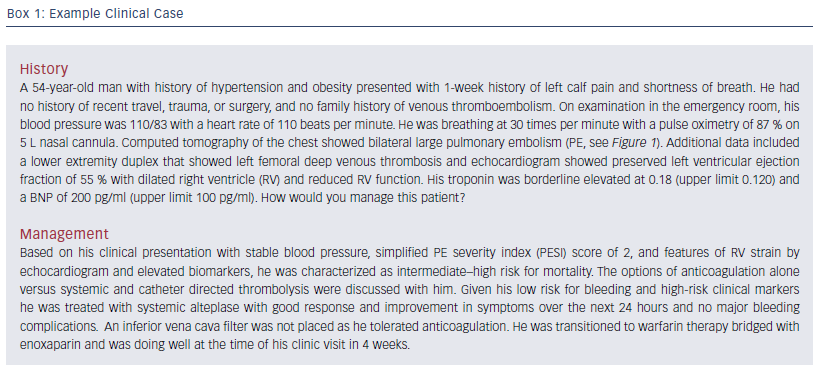
- A 54-year-old man with a myocardial infarction is treated with an antiplatelet drug that blocks the Platelet P2Y12 receptor.
Fibrinolytic Therapy
Fibrinolytic therapy is designed to dissolve clots and is pivotal in cases of acute MI, especially when PCI is unavailable. Some of the main agents include:
- Alteplase (rt-PA): Highly fibrin-specific.
- Reteplase: Less fibrin-specific but more cost-effective.
- Urokinase: Used for peripheral intravascular thrombus and occluded catheters.
- Streptokinase: Binds plasminogen to form an active enzyme complex.
Clinical Implications
Patients with acute STEMI should receive coronary reperfusion therapy. Fibrinolytic therapy, if administered quickly, can significantly improve cardiovascular outcomes.
Contraindications
For instance, a man presenting with acute hemiparesis and high blood glucose might have contraindications to tPA due to a recent stroke.