Mechanisms of Arrhythmia
Mechanisms of Arrhythmia
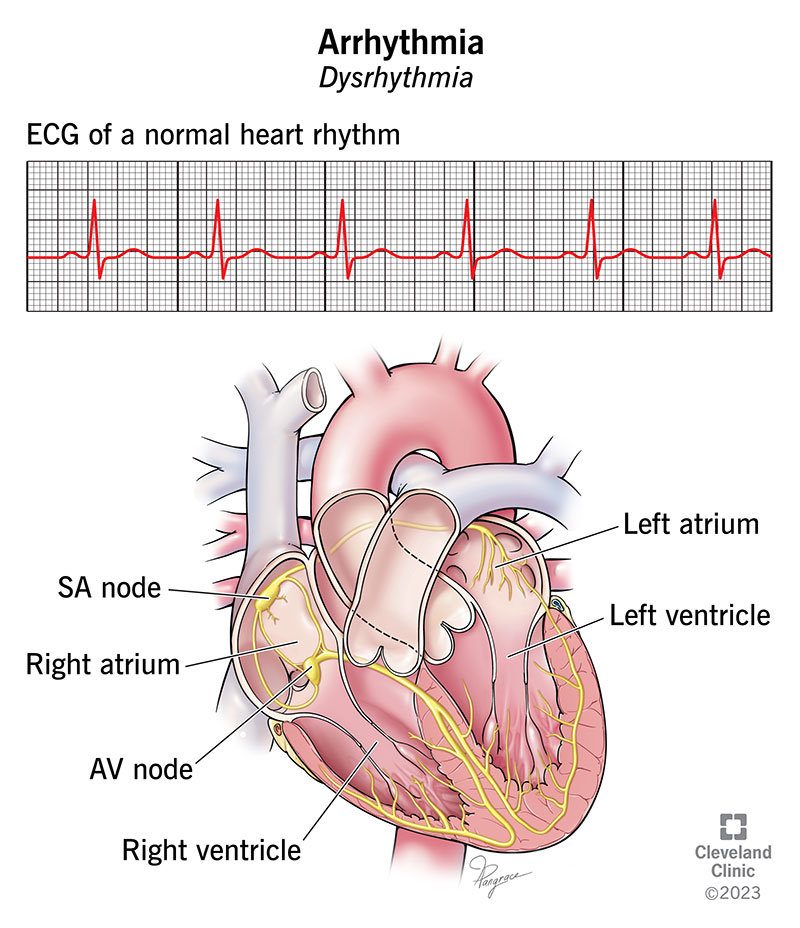
Normal Sinus Rhythm
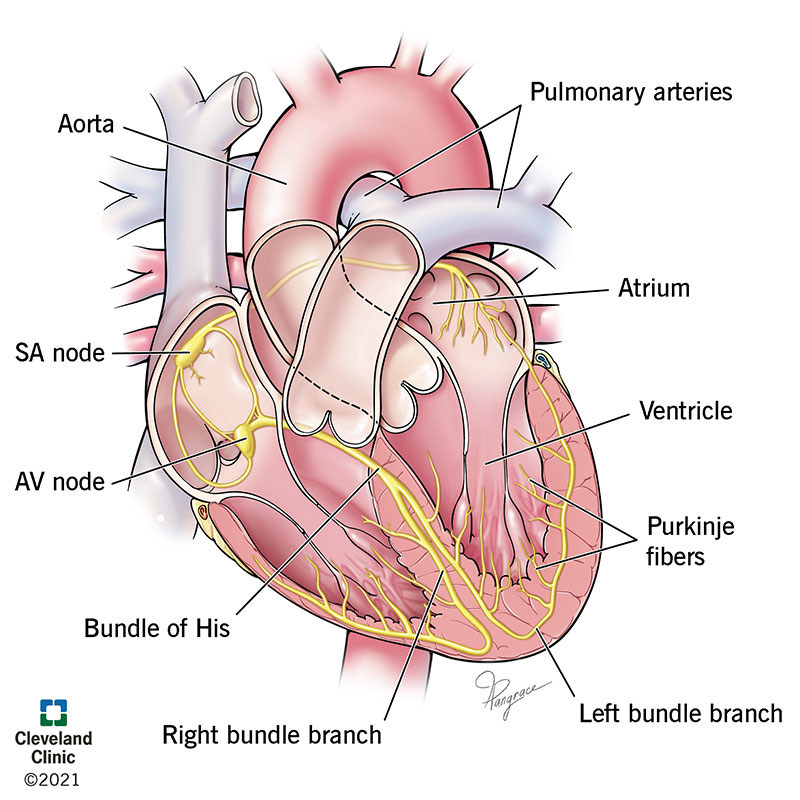
Components of the Cardiac Conduction System:
- SA node - The primary pacemaker of the heart, located in the right atrium.
- AV node - Acts as a gateway that slows the conduction before the signal passes to the ventricles.
- Purkinje fibers - Spread the conduction throughout the ventricles.
Electrocardiogram (ECG) Phases:
- P wave: Atrial excitation
- PR interval: AV conduction
- QRS complex: Ventricular excitation, Phase 0 (Na+ influx)
- QT interval: Total Time of Ventricular Excitation & Recovery, Phase 3 (K+ efflux)
- T wave: Ventricular repolarization

Types of Arrhythmia
- Bradycardia (slow): Results from slow heart rates originating from the atria or AV node.
- Tachycardia (fast): Results from fast heart rates originating from the ventricles.

Causes of Arrhythmias
Altered Impulse Formation:
Altered Automaticity: Can be of the SA node or latent pathways influenced by the autonomic nervous system.
- Sympathetic activation increases cAMP, enhancing pacemaker currents in nodal cells.
- ↑ cAMP → ↑ pacemaker currents
- Parasympathetic activation via ACh can suppress the SA node.
- Ph4 slope, Threshold Potential (TP), and Maximum Diastolic Potential (MDP) determine cell firing rates.
- Sympathetic activation increases cAMP, enhancing pacemaker currents in nodal cells.
Abnormal Automaticity: Cells outside of the regular conduction system spontaneously depolarize, often due to injury-caused leaky membranes.
- Can initiate ectopic beats or rhythms.
Triggered Activity: Due to abnormal depolarizations triggered by previous action potentials.
- Early Afterdepolarizations (EAD): Interrupt normal repolarization, often associated with Long QT syndrome.
- Delayed Afterdepolarizations (DAD): Caused by high intracellular calcium levels.
Altered Impulse Conduction:
Conduction Block: Impulse blocked by an unexcitable region. Can be transient or permanent, unidirectional or bidirectional.
- Functional: During refractory periods.
- Structural: Due to ischemia, fibrosis (scarring), or inflammation.
- AV block: Most common type.
Reentry Circuits: Electrical impulses circulate repeatedly around a reentry circuit, often associated with unidirectional conduction blocks.
- Requires continuously excitable tissue, often seen with myocardial scars.
- Usually leads to tachycardia.
AV nodal reentry: A specific type of reentry involving the AV node, which can generate a large reentry loop leading to tachycardia.
Specific Arrhythmia Examples:
Wolff-Parkinson-White Syndrome (WPW):
- Abnormal accessory conduction pathway from atria to ventricles (Bundle of Kent) bypasses the rate-slowing AV node.
- Characterized by a delta wave on ECG, with widened QRS complex and shortened PR interval.
- Can lead to life-threatening tachycardia through reentry circuits.
Basis for Antiarrhythmic Therapy:
- Eliminate Increased Automaticity:
- Decrease Phase 4 slope, increase Threshold Potential (TP), decrease Maximum Diastolic Potential (MDP).
- Eliminate Triggered Activity:
- Shorten action potential duration (EAD) or reduce calcium overload (DAD).
- Interrupt Reentrant Circuits:
- Increase refractory periods, reduce premature beats.
Mechanisms of Arrhythmia Development
Bradyarrhythmias (Decreased Firing Rate):
- Decreased Automaticity: Often caused by parasympathetic stimulation or other factors reducing phase 4 depolarization.
Tachyarrhythmias (Increased Firing Rate):
- Enhanced Automaticity: Can be due to sympathetic stimulation or ectopic foci acquiring pacemaker activity.
- Triggered Activity: Due to prolonged action potential duration (EAD) or intracellular calcium overload (DAD).
- Reentry Circuits: Unidirectional block with slowed conduction.
- Functional: May involve atrial fibrillation, polymorphic VT, ventricular fibrillation.
- Anatomical: Involves atrial flutter, AV nodal reentrant tachycardia, VT related to scar tissue.
Note: Treatment strategies for arrhythmias often involve addressing the underlying abnormality, be it enhanced automaticity, triggered activity, or reentry circuits.