Stable Ischemic Heart Disease
Stable Ischemic Heart Disease
Learning Objectives
Define Ischemia:
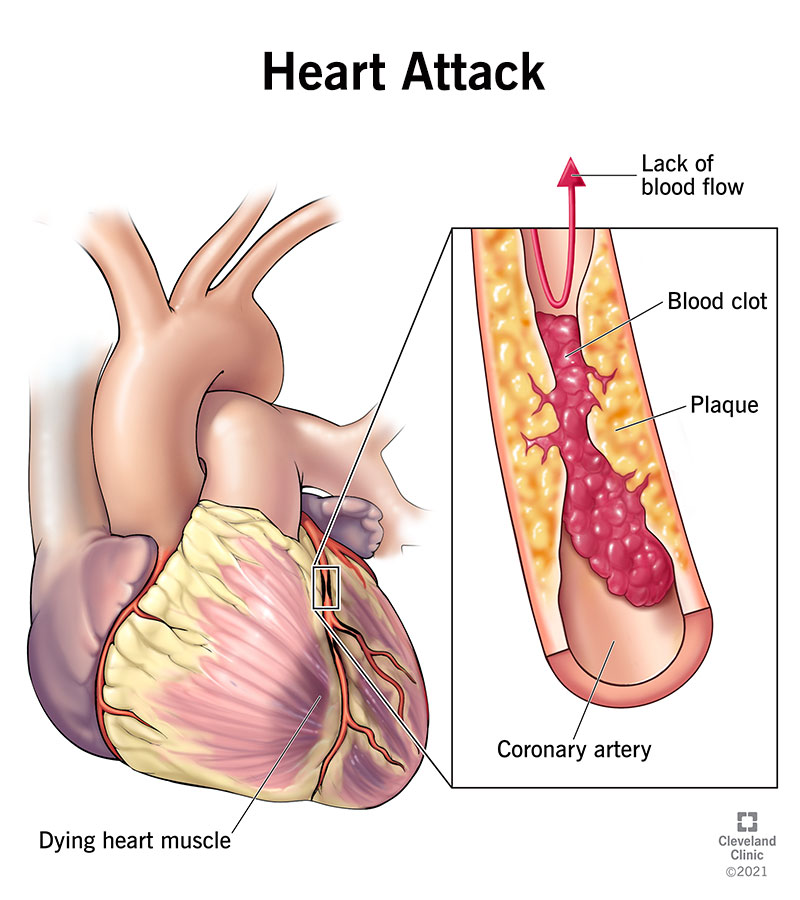
Ischemia refers to a condition where there is an inadequate supply of blood to a tissue or organ, often due to obstruction or narrowing of arteries, leading to a deficiency of oxygen and nutrients. In the context of the heart, ischemia typically refers to reduced blood flow to the heart muscle (myocardium), often caused by coronary artery disease (CAD).
Identify the Principles of Normal and Abnormal Blood Flow in the Coronary Microcirculation:
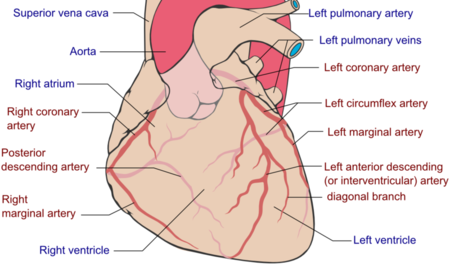
- Normal Blood Flow: In a healthy heart, the coronary arteries deliver oxygen-rich blood to the myocardium. The microcirculation involves the arterioles, capillaries, and venules that provide precise regulation of blood flow to meet the oxygen demands of the heart, particularly during exertion. This process is mediated by autoregulation mechanisms that control vasodilation and vasoconstriction.
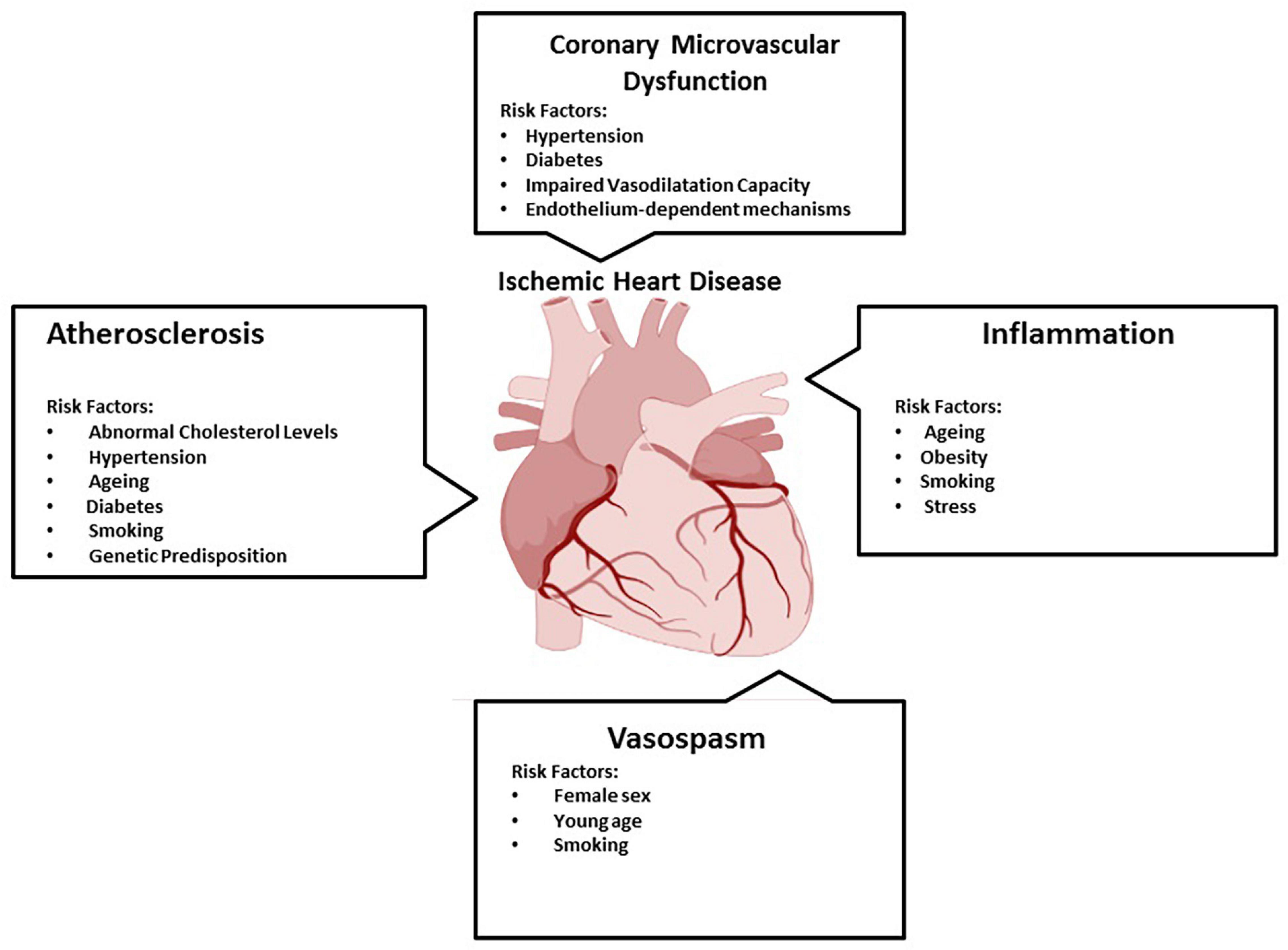
- Abnormal Blood Flow: Abnormalities in blood flow occur when the coronary arteries are narrowed or blocked, typically due to atherosclerosis (plaque buildup). This leads to reduced blood supply to the myocardium (ischemia). Factors such as endothelial dysfunction, vascular inflammation, and vasospasm can also impair microcirculatory function, further complicating blood flow regulation and oxygen delivery.
Discuss the Clinical Presentation and Exam Findings of Stable Ischemic Heart Disease (SIHD):
- Clinical Presentation: Stable ischemic heart disease (also known as stable angina) typically presents with chest pain or discomfort, often described as pressure, tightness, or heaviness, especially during physical exertion or emotional stress. This pain is usually relieved by rest or nitroglycerin. Patients may also experience referred pain in the neck, jaw, shoulder, or arm, as well as shortness of breath, fatigue, or nausea.
- Physical Exam Findings: Physical exam findings in stable ischemic heart disease can be normal, especially between episodes of chest pain. However, during an ischemic episode, a patient may appear diaphoretic (sweaty) or anxious. Auscultation may reveal abnormal heart sounds such as an S4 gallop, and in severe cases, there may be signs of heart failure (e.g., peripheral edema or rales). Additionally, the presence of risk factors like hypertension, diabetes, or obesity may be noted.
Describe the Management of Stable Ischemic Heart Disease:
- Lifestyle Modifications: Management begins with lifestyle changes, such as smoking cessation, dietary improvements (low-fat, low-sodium diet), weight management, and regular physical activity. These modifications aim to reduce cardiovascular risk factors.
- Medications:
- Antiplatelet Agents: Aspirin or other antiplatelet medications (e.g., clopidogrel) are used to reduce the risk of thrombotic events.
- Antianginal Medications: These include nitrates (e.g., nitroglycerin), beta-blockers, calcium channel blockers, and ranolazine to relieve angina by reducing myocardial oxygen demand and improving coronary blood flow.
- Statins: Statins are prescribed to lower cholesterol levels and stabilize atherosclerotic plaques.
- ACE Inhibitors or ARBs: These may be used to manage hypertension and protect against further cardiovascular events.
- Revascularization: In cases where medical therapy is insufficient, revascularization procedures, such as percutaneous coronary intervention (PCI) with stenting or coronary artery bypass grafting (CABG), may be performed to restore adequate blood flow to the heart.
- Monitoring and Follow-up: Patients with SIHD require regular monitoring, including exercise stress tests, imaging studies, and ongoing assessment of risk factors like blood pressure, cholesterol, and diabetes control.
Define Ischemia:
Ischemia refers to a condition where there is an inadequate supply of blood to a tissue or organ, often due to obstruction or narrowing of arteries, leading to a deficiency of oxygen and nutrients. In the context of the heart, ischemia typically refers to reduced blood flow to the heart muscle (myocardium), often caused by coronary artery disease (CAD).
Identify the Principles of Normal and Abnormal Blood Flow in the Coronary Microcirculation:
- Normal Blood Flow: In a healthy heart, the coronary arteries deliver oxygen-rich blood to the myocardium. The microcirculation involves the arterioles, capillaries, and venules that provide precise regulation of blood flow to meet the oxygen demands of the heart, particularly during exertion. This process is mediated by autoregulation mechanisms that control vasodilation and vasoconstriction.
- Abnormal Blood Flow: Abnormalities in blood flow occur when the coronary arteries are narrowed or blocked, typically due to atherosclerosis (plaque buildup). This leads to reduced blood supply to the myocardium (ischemia). Factors such as endothelial dysfunction, vascular inflammation, and vasospasm can also impair microcirculatory function, further complicating blood flow regulation and oxygen delivery.
Discuss the Clinical Presentation and Exam Findings of Stable Ischemic Heart Disease (SIHD):
- Clinical Presentation: Stable ischemic heart disease (also known as stable angina) typically presents with chest pain or discomfort, often described as pressure, tightness, or heaviness, especially during physical exertion or emotional stress. This pain is usually relieved by rest or nitroglycerin. Patients may also experience referred pain in the neck, jaw, shoulder, or arm, as well as shortness of breath, fatigue, or nausea.
- Physical Exam Findings: Physical exam findings in stable ischemic heart disease can be normal, especially between episodes of chest pain. However, during an ischemic episode, a patient may appear diaphoretic (sweaty) or anxious. Auscultation may reveal abnormal heart sounds such as an S4 gallop, and in severe cases, there may be signs of heart failure (e.g., peripheral edema or rales). Additionally, the presence of risk factors like hypertension, diabetes, or obesity may be noted.
Describe the Management of Stable Ischemic Heart Disease:
- Lifestyle Modifications: Management begins with lifestyle changes, such as smoking cessation, dietary improvements (low-fat, low-sodium diet), weight management, and regular physical activity. These modifications aim to reduce cardiovascular risk factors.
- Medications:
- Antiplatelet Agents: Aspirin or other antiplatelet medications (e.g., clopidogrel) are used to reduce the risk of thrombotic events.
- Antianginal Medications: These include nitrates (e.g., nitroglycerin), beta-blockers, calcium channel blockers, and ranolazine to relieve angina by reducing myocardial oxygen demand and improving coronary blood flow.
- Statins: Statins are prescribed to lower cholesterol levels and stabilize atherosclerotic plaques.
- ACE Inhibitors or ARBs: These may be used to manage hypertension and protect against further cardiovascular events.
- Revascularization: In cases where medical therapy is insufficient, revascularization procedures, such as percutaneous coronary intervention (PCI) with stenting or coronary artery bypass grafting (CABG), may be performed to restore adequate blood flow to the heart.
- Monitoring and Follow-up: Patients with SIHD require regular monitoring, including exercise stress tests, imaging studies, and ongoing assessment of risk factors like blood pressure, cholesterol, and diabetes control.

Epidemiology
- More than 655,000 Americans died of heart disease in 2017 (per CDC).
- The term is often used interchangeably with coronary artery disease (CAD).
- Not all ischemia is related to atherosclerosis.

Spectrum of Ischemic Heart Disease
- Asymptomatic IHD (SIHD, PCI/CABG)
- Asymptomatic, New-Onset Chest Pain Without Known IHD
- Stable Angina or Low-Risk UA
- Acute Coronary Syndromes (UA/NSTEMI, STEMI, PCI/CABG)
- Sudden Cardiac Death (VA-SCD)
What is ischemia?
- Ischemia is defined as a condition of inadequate blood flow to a region.
- It can be either episodic or persistent.
- It is most commonly caused by a fixed atherosclerotic lesion in the epicardial coronary arteries.
- Can occur with vasospastic disease, hypotension, etc. (with no obstructive disease).
The Ischemic Cascade
- ECG abnormalities
- Anginal chest pain
- Regional wall motion abnormalities
- Contractility abnormalities
- Relaxation disturbances
- Metabolic abnormalities
- Reversible myocardial changes
- Irreversible myocardial damage
- 20-30 min coronary artery occlusion
Coronary Artery Microcirculation
- Epicardial arteries (>500 um)
- Pre-arterioles (500-200 um)
- Arterioles (<200 um)
- Capillaries (<10 um)
The subendocardium is particularly vulnerable to ischemia and is represented by ST depression
- Below 70% stenosis, distal arteriole dilation can accommodate both resting and exertional states
- Above roughly 70% stenosis, distal arteriole dilation can accommodate resting but not exertional states
- Exertional chest pain that goes away after rest or nitro
- Above roughly 90% stenosis, distal arterioles are fully dilated but can’t compensate for the extreme stenosis
- Pain at rest, cell death

Causes of Ischemia
- Stunning
- Contractile dysfunction after ischemia
- No necrosis
- Low ATP
- Slowly reversible
- Hibernation
- Contractile dysfunction during low coronary flow
- No necrosis
- Normal phosphorus metabolites
- Quickly reversible
Non-Atherosclerotic Causes of Ischemia
- Hypotension (decreased perfusion pressure)
- Severe anemia (marked decrease in blood oxygen content)
- Rapid tachyarrhythmias
- Marked hypertension

Prinzmetal Angina (Vasospasm)
- Non-significant stenosis
- Sub-occlusive coronary spasm
- Temporary reduction in coronary flow
- Treatment goal: relax vessel/reverse spasm
- Treat with vasodilators—calcium channel blocker and/or nitrates
Major Risk Factors for Cardiovascular Disease
- Unhealthy Lifestyle
- Cigarette smoking
- Physical inactivity
- Diet high in fat
- Obesity
- High Risk Diseases
- Hypertension
- Diabetes
- Hyperlipidemia
- End Organ Damage
- Heart disease
- Stroke
- Peripheral artery disease
- Chronic kidney disease
- Eye sight failure
- Non-Modifiable Factors
- Age
- Family history of premature coronary artery disease (CAD)