Bacterial Endocarditis and Rheumatic Fever
Title: Bacterial Endocarditis and Rheumatic Fever
Learning Objectives
- Know the difference between acute and subacute endocarditis with respect to the most prominent causal organisms, clinical presentation, and clinical approach.
- Know relevant differences between native valve endocarditis, prosthetic valve endocarditis, and endocarditis associated with intravenous drug abuse.
- Know the key steps in the pathogenesis of infective endocarditis (e.g., how does it happen?).
- Know risk factors for the development of infective endocarditis.
- Know the general principles and underlying logic of the Duke diagnostic criteria.
- Know the pathogenic basis for the development of rheumatic fever and the principles of its medical management.
- Know the general principles and underlying logic of the Jones diagnostic criteria.
Carditis: Inflammatory Diseases of the Heart

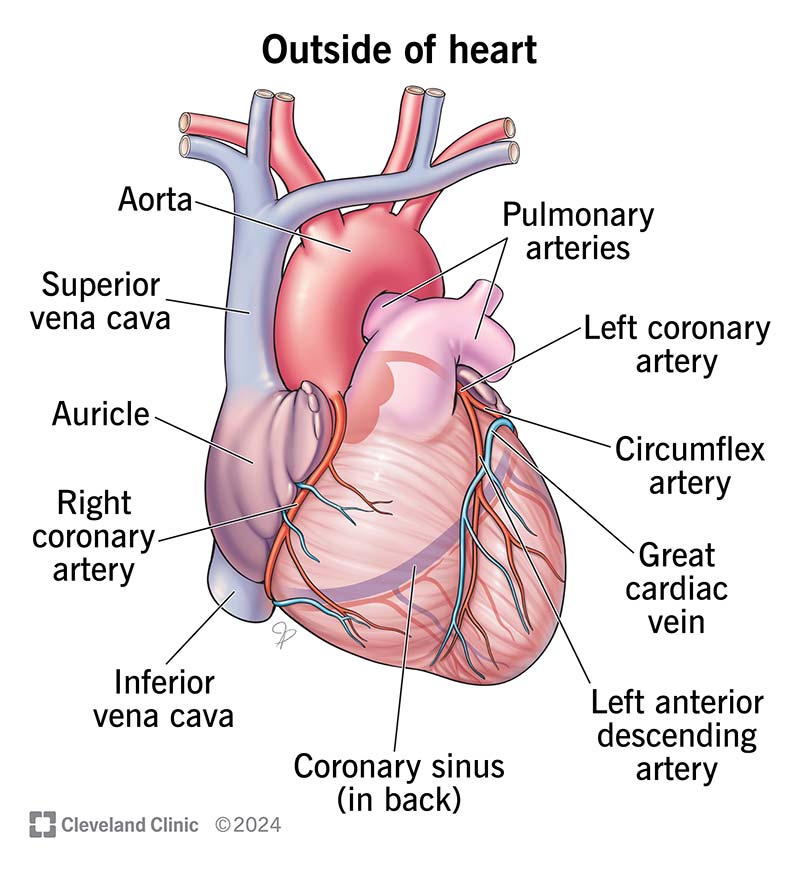
Pericarditis: - Inflammation on the outside of the heart - Etiology: Viral >>> bacterial >> fungal - Often idiopathic
Myocarditis: - Inflammation of the heart muscle - Etiology: Viral >> bacterial > fungal - Sometimes autoimmune
Endocarditis: - Inflammation of the endocardium (innermost lining of the heart) - Lines all chambers and valves - Continuous with vessels leaving the heart - Etiology: Bacterial >>>>> fungal > viral - Can be a life-threatening medical emergency requiring empiric antibiotic therapy - 100% mortality without antibiotic therapy (20-25% even with appropriate therapy)
Forms of Bacterial Endocarditis

Acute Endocarditis: - Often occurs on structurally normal valves - Can cause extensive damage to cardiac structures - Metastatic (dissemination to other sites) - Rapid course (untreated = death in days to weeks) - Treatment often requires surgery - Most common pathogen: Staphylococcus aureus - Sometimes Streptococcus pyogenes, but far less common - Much more likely to require empiric therapy, often using multiple antibiotics
Subacute Endocarditis: - Occurs primarily on damaged valves - Causes little structural damage to the valve - Rarely metastatic - More indolent course (weeks to months before diagnosis) - Often resolved without surgery - Most common pathogens: - viridans streptococci - S. epidermidis (coagulase negative) - Rarely need to treat empirically and in fact shouldn’t pending confirmed bacteriological results
Other Considerations
Native Valve Endocarditis (NVE): - Staphylococcus aureus, viridans streptococci - Native valve does not mean normal valve... - Most common predisposition: mitral valve prolapse
Prosthetic Valve Endocarditis (PVE): - Same bacteria, but add coagulase-negative staphylococci (e.g., S. epidermidis)
IV Drug Users: - Often involves the right side of the heart (tricuspid valve) - Most common pathogens: Staphylococcus aureus, Oral pathogens (due to contamination of needles with saliva, often involves Gram-negative HACEK)
Causes of Bacterial Endocarditis: Summary

- HACEK: Haemophilus, Actinobacillus, Cardiobacterium, Eikenella, and Kingella
- All are Gram-negative (important with respect to empiric therapy)
- Particularly problematic in IV drug users
- Gram-positive cocci (Staphylococcus, Streptococcus, and Enterococcus account for ~90% of all cases)
- Most prominent in acute cases: Staphylococcus aureus
- Most prominent in subacute cases: viridans streptococci
- Prosthetic valve strong risk factor for S. epidermidis
- Everything else is relatively rare and causes subacute endocarditis