Microcirculation, Capillary Exchange, and the Lymphatic System
Microcirculation, Capillary Exchange, and the Lymphatic System

Capillary Structures Critical to Function
The microcirculation system is vital for the transport of nutrients to tissues and the removal of waste products. It comprises over 10 billion capillaries, with a surface area of 500-700 square meters, responsible for the exchange of solutes and fluids. Capillaries are composed of a unicellular layer of endothelial cells surrounded by a basement membrane, with diameters ranging from 4 to 9 microns. Various types of capillaries include continuous capillaries (common in adipose, muscle, and brain tissues) and fenestrated capillaries (found in renal glomeruli, endocrine glands, intestinal villi, and exocrine pancreas).
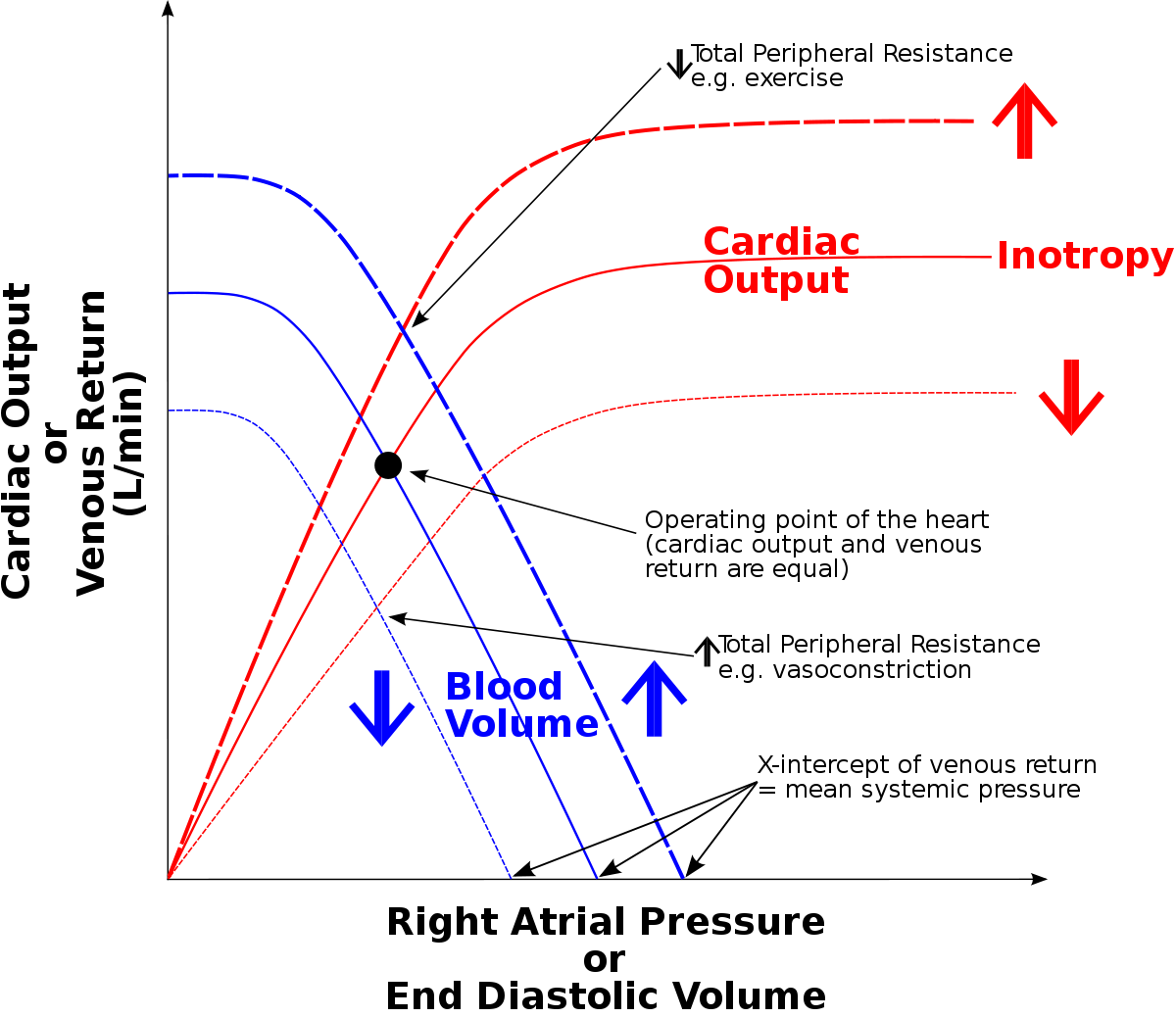
Capillary Filtration and Reabsorption Forces
Capillary filtration and reabsorption are determined by four critical forces, often described by the Starling equation:
- Capillary Hydrostatic Pressure (Pc): Forces fluid outward through the capillary membrane.
- Interstitial Fluid Pressure (Pif): Opposes filtration when its value is positive.
- Plasma Colloid Osmotic Pressure (πp): Opposes filtration, causing osmosis of water inward through the membrane.
- Interstitial Fluid Colloid Pressure (πif): Promotes filtration by causing osmosis of fluid outward through the membrane.
The net filtration pressure (NFP) can be calculated as:
NFP= Pc - Pif - πp + πif
Solute and Fluid Exchange Across Capillaries
The primary method of substance transfer between plasma and interstitial fluid is by diffusion. Lipid-soluble substances (e.g., CO2, O2) diffuse directly through the cell membrane, while lipid-insoluble substances (e.g., H2O, Na, Cl, glucose) cross via intercellular clefts. Differences in concentration across the capillary enhance diffusion.
Relative Permeability of Capillary Pores to Different-Sized Molecules- Water (Molecular Weight: 18) - Permeability: 1.00
- NaCl (58.5) - Permeability: 0.96
- Urea (60) - Permeability: 0.8
- Glucose (180) - Permeability: 0.6
- Sucrose (342) - Permeability: 0.4
- Insulin (5000) - Permeability: 0.2
- Myoglobin (17,600) - Permeability: 0.03
- Hemoglobin (69,000) - Permeability: 0.01
- Albumin (69,000) - Permeability: 0.001
Microcirculation and Clinical Significance
Microcirculation is critical for tissue nutrient supply and waste removal. Disruption of microcirculatory perfusion is linked to severe organ failure and poor outcomes, notably in conditions such as hemorrhagic, cardiogenic, and septic shock. For example, in sepsis, increased capillary permeability and vasodilation lead to vascular leakage, hypovolemic shock, reduced cardiac output, and ultimately end-organ failure.

The Lymphatic System
The lymphatic system is an accessory route for fluid and protein flow from interstitial spaces to the blood, playing a vital role in preventing edema. It is derived from interstitial fluid that flows into the lymphatics, and it also serves as a major route for nutrient absorption from the GI tract. Crucially, it regulates immune responses, drains excess interstitial fluid, and absorbs lipids from the intestine.
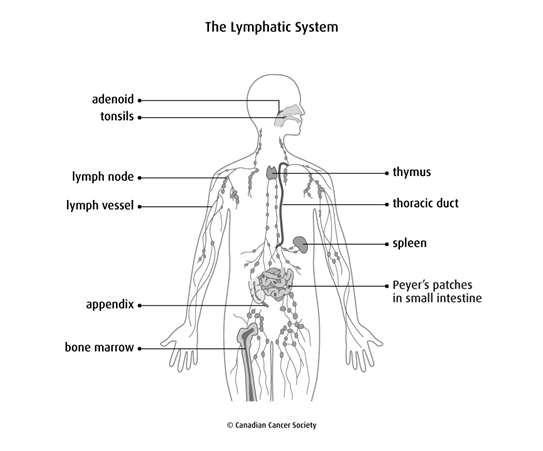
Determinants of Lymph Flow
- The degree of activity of the lymphatic pump, including smooth muscle contraction and external compression, contributes to lymphatic pumping.
Edema results from several mechanisms:
- Increased Capillary Pressure: Often due to conditions like congestive heart failure.
- Decreased Plasma Proteins are seen in nephrotic syndrome or liver failure, leading to excess fluid outflow into the interstitium.
- Increased Capillary Permeability: Conditions such as infections or burns cause fluid outflow into the interstitium.
Summary of Clinical Case
A 66-year-old male with a history of myocardial infarction presents with dyspnea on exertion and swollen feet and ankles. Physical examination reveals elevated jugular venous pressure and pitting edema of bilateral lower extremities. The most likely explanation is increased capillary pressure secondary to congestive heart failure, leading to fluid backup.
Pharmacological interventions may include diuretics for symptom relief and ACE inhibitors, ARBs, or beta-blockers to modify disease progression. Lifestyle changes, such as sodium restriction, are also recommended.