Heart Failure: Foundations and Frameworks
Heart Failure: Foundations and Frameworks

What Is Heart Failure?
Heart failure (HF), sometimes referred to as congestive heart failure (CHF), is a syndrome in which the heart is unable to pump sufficient blood to meet the needs of the body.
HF is a leading cause of death and diminished quality of life throughout the world, affecting at least 6 million people in the United States (2% of the population) and 23 million worldwide. Fifty percent of those diagnosed with clinical heart failure are dead within 5 years, and the prevalence increases with age. Patients with HF most commonly have ischemic (coronary artery) disease along with comorbidities including diabetes, hypertension, and smoking, but there are many other causes of HF as well.
You can categorize HF into groups by function (systolic or nonsystolic), location (left- or right-sided), or by a specific pathologic cause. In this brick we will introduce these categories to set the stage for your further reading.
:max_bytes(150000):strip_icc()/systolic-vs-diastolic-heart-failure-5181815_V2-a8f3d422327248cb9f26fe91ab321852.jpg)
Is It Systolic or Diastolic Heart Failure?
In this section, we will classify heart failure as systolic or diastolic (also called nonsystolic).
Systolic Heart Failure
Systolic heart failure occurs when the ventricles are unable to pump blood adequately to meet the needs of the body. It is characterized by: - Decreased contractility: the inability of the myocytes (heart muscle fibers) to shorten and cause contractions. - Reduced stroke volume: the amount of blood ejected during each cycle. - Reduced ejection fraction (EF): the fraction of blood ejected from a ventricle with each contraction. Some experts call systolic heart failure as "heart failure with reduced ejection fraction" to emphasize the key physiology. - Increased end-diastolic volume (EDV): the volume of blood in the ventricle at the end of the filling period (diastole) but before systole begins.
The sequence begins with decreased contractility (due to ischemia, viruses, toxins, etc.), which reduces the stroke volume and ejection fraction. Because the heart cannot pump blood adequately, there are increases in EDV, left ventricular and left atrial pressures, and pulmonary vein and capillary pressures. This leads to fluid moving into the alveoli of the lungs, and resultant pulmonary congestion and dyspnea (cardiogenic pulmonary edema).
What causes systolic HF? Ventricular dilation due to diseased myocytes is generally associated with systolic HF and is most often caused by ischemic heart disease (e.g., myocardial infarction). Ventricle dilation can also be caused by dilated cardiomyopathy due to viruses (e.g., Echo virus, COVID-19, and HIV) or toxins (alcohol, cocaine, or the chemotherapy drug doxorubicin).
Hypothyroidism can cause systolic HF by lowering the pulse and contractility (with normal cardiomyocytes). This condition is easily corrected by treatment with a thyroid hormone.
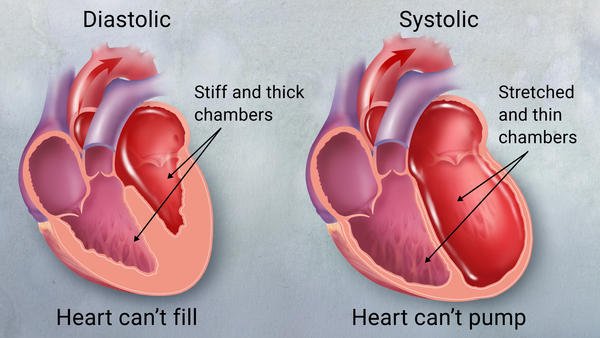
Diastolic Heart Failure
Diastolic heart failure (also called nonsystolic HF or heart failure with preserved ejection fraction) is the inability of the ventricle to adequately relax and fill with blood. The contractility of the ventricle is maintained, unlike systolic HF. It is characterized by the following: - Decreased ventricular compliance (i.e., increased stiffness) - Reduced or normal EDV - Reduced stroke volume - Preserved EF (this is why diastolic heart failure is also referred to as “heart failure with preserved ejection fraction")
How does this all fit together? Compliance is the ability of the heart muscle fibers to lengthen in response to pressure of the ventricle (compliance = change in volume divided by change in pressure [C = ΔV / ΔP]). Decreased compliance impairs ventricular filling and decreases the EDV. The reduced EDV reduces ventricular stretch and so reduces preload. The reduced preload reduces the stroke volume. But since both EDV and stroke volume (SV) are decreased proportionately, the ejection fraction (SV / EDV) is unchanged, reflecting the unchanged myocardial contractility.
What are the possible causes of diastolic HF? Hypertension, aortic stenosis, hypertrophic obstructive cardiomyopathy (a genetic disorder), and severe renal disease (end-stage kidney disease) can all cause diastolic HF. These conditionsouncil can all cause the cardiac muscle to hypertrophy. As the wall becomes thicker, the area inside the ventricle becomes smaller.
:max_bytes(150000):strip_icc()/VWH-JessicaOlah-LeftvsRightSidedHeartFailure-Standard-33b2b8e3250644d9a5d61024b8144c18.jpeg)
Are the Symptoms Left-Sided or Right-Sided?
HF symptoms can be distinguished as either left-sided or right-sided and, depending on which side of the heart is affected, the symptoms can vary.
Left-Sided Heart Failure
We can divide the findings of left-sided HF into “forward” and “backward” signs and symptoms. When the left ventricle doesn’t pump properly, blood does not travel forward into the circulation at an adequate rate, depriving the organs of blood (and oxygen).
This causes symptoms of “forward” failure, which leads to tachycardia, dizziness, confusion, and reduced renal perfusion causing reduced glomerular filtration (GFR) and often increased sodium and water retention (edema).
But, in addition, the heart cannot empty properly, so blood builds up behind the failed ventricles in the lungs and/or the venous system. This is “backward” failure. This condition can be detected by lung crackles on exam and can lead to congestion of the pulmonary vasculature, resulting in dyspnea, cough, orthopnea (shortness of breath when lying down), and paroxysmal nocturnal dyspnea (waking up breathless from sleep).
Left-sided HF is caused by the same list of diseases mentioned above for systolic and diastolic HF.
Right-Sided Heart FailureIn right heart failure, blood from the right ventricle backs up into the systemic circulation, leading to hepatomegaly, jugular venous distention, and peripheral edema.
The most common trigger of right-sided HF is actually left-sided HF, so right heart failure only uncommonly occurs in isolation. This is partly because the causes of left-sided HF are more common. So how exactly does dysfunction on the left side lead to ventricular dysfunction on the right side of the heart?
Since left-sided HF leads to pulmonary congestion, this congestion eventually backs up enough to put excessive pressure and volume in the right heart. Being the weaker chamber, the right ventricle cannot overcome the increased pressure and volume brought on by pulmonary congestion, and ultimately right-sided ventricular dysfunction and failure result.
Less commonly, some types of right heart failure can occur without left heart failure: - A specific type of genetic HF limited to the right ventricle is arrhythmogenic right ventricular cardiomyopathy. - On rare occasions, primary lung disease causes elevated capillary pressure in the lung vessels (pulmonary hypertension) that can cause backup of blood into the right ventricle, causing isolated failure of the right heart. This condition is called cor pulmonale.
What Are the Pathologic Types of Heart Failure?
The final way we can classify HF is by pathologic findings, which define what is seen in the histology of the ventricle if a biopsy is done (which is not usually the case). In the United States, most patients have abnormal myocardium secondary to causes like coronary artery (ischemic heart disease), valve disease, congenital heart lesions, or prolonged hypertension. However, primary disease of the myocardium also causes heart failure.
The four types of “cardiomyopathy” (primary disease of the myocardium) include:
- Dilated cardiomyopathy: This is the most common cardiomyopathy. The ventricles are thinned and lose contractility, usually due to viral infection, myocarditis, or toxins (e.g., heavy alcohol consumption or the chemotherapy drug doxorubicin). Dilated cardiomyopathy causes systolic HF and can affect both ventricles.
- Hypertrophic cardiomyopathy: This is an uncommon genetic disorder that leads to left ventricle (LV) hypertrophy and diminished ventricular outflow, causing diastolic HF, dyspnea, and arrhythmias in young adults.
- Restrictive cardiomyopathy: In this uncommon disorder, the heart has a stiff, poorly functioning myocardium, caused either by fibrosis (e.g., due to systemic sclerosis or radiation damage) or infiltrative disease (e.g., sarcoidosis, amyloidosis).
- Arrhythmogenic right ventricular cardiomyopathy: This rare genetic disorder causes fatty infiltration of the right ventricle, leading to arrhythmias and systolic right heart failure.