Circulatory Shock: Diagnosis and Management
Circulatory Shock
The Equation of Life
The primary equation that guides the understanding of circulatory shock is the Equation of Life:
DO2 = CO x CaO2
Where:
- DO2: Delivery of O2 (mL/min)
- CO: Cardiac output (L/min)
- CaO2: Arterial O2 content (mL/L)
Cardiac Output (CO) can be broken down into:
CO = HR x SV
Where:
- HR: Heart rate (beats/min)
- SV: Stroke volume (L)
Stroke volume (SV) itself is dependent on four factors:
- Preload (aka venous return): The amount of filling of the ventricle at end-diastole.
- Contractility: The force generated by the ventricle during systole.
- Afterload (aka systemic vascular resistance - SVR): The force against which the ventricle must work to eject blood during systole.
- Lusitropy: Myocardial relaxation during diastole.
Arterial O2 Content (CaO2) formula:
CaO2 = [1.34 x Hgb x (SaO2/100)] + [0.003 x PaO2]
Where:
- Hgb: Hemoglobin (g/dL)
- SaO2: Arterial O2 saturation (%).
- PaO2: Arterial partial pressure of O2 (mmHg).

Types of Shock
Shock is defined as an acute, life-threatening disorder of tissue perfusion that, if untreated, can lead to death. The types of shock are classified as follows:
- Hypovolemic Shock: Primary problem is a pre-load deficit. This can be due to hemorrhagic causes (e.g., trauma, surgical, massive GI bleed) or non-hemorrhagic causes (e.g., dehydration, vomiting/diarrhea, osmotic diuresis, insensible losses, sepsis).
- Cardiogenic Shock: Primary problem is impaired contractility and/or lusitropy. Causes include myocarditis, cardiomyopathy, low cardiac output syndrome after cardiopulmonary bypass, arrhythmias, severe valvular disorders, metabolic derangements/disorders, and ischemia from coronary disorders.
- Obstructive Shock: Primary problem is cardiac output (CO) obstruction leading to impaired contractility and/or lusitropy. Causes include tension pneumothorax, cardiac tamponade, mediastinal mass, massive pulmonary embolus, and certain forms of congenital heart disease.
- Distributive Shock: Primary problem is a derangement in vascular tone leading to decreased SVR (systemic vascular resistance). Causes include anaphylaxis, spinal cord trauma with neurogenic shock, and sepsis.
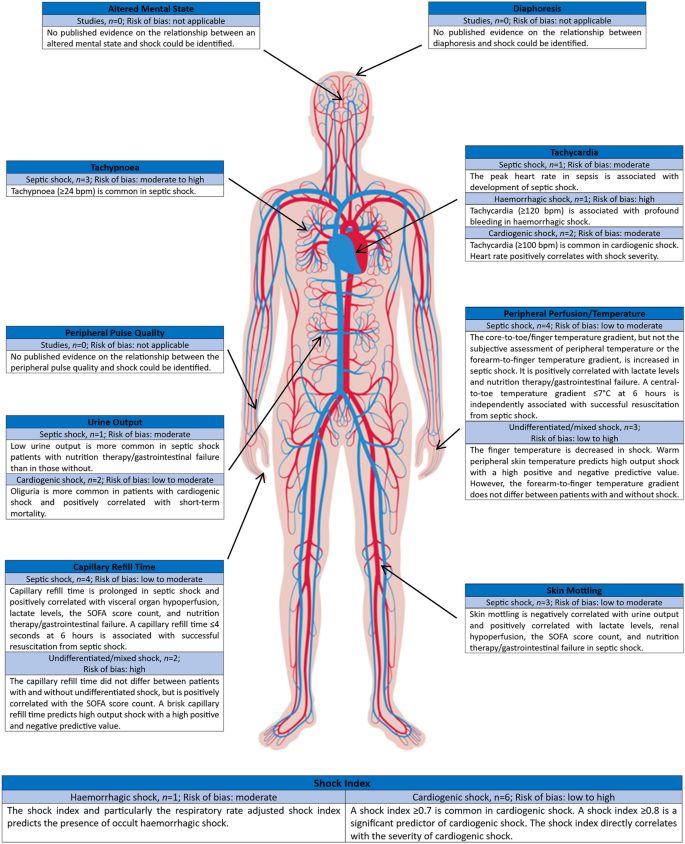
Recognition of Shock
Recognizing a patient in shock involves noting clinical signs that indicate poor perfusion and tissue oxygenation. These signs can include:
- Pulse rate: Tachycardia is often an early sign.
- Respiratory rate: Tachypnea may be present.
- Skin: Cool, clammy, or mottled skin can indicate hypovolemic or cardiogenic shock; warm, flushed skin may indicate distributive shock.
- Capillary refill: Delayed capillary refill time (more than 2 seconds).
- Mental status: Altered mental states such as confusion, lethargy, or unresponsiveness.
- Urine output: Decreased urine output can indicate reduced renal perfusion.
Treatment of Shock
Initial Steps
- Oxygen Supply - Ensure adequate oxygen delivery by providing supplemental oxygen.
- Intravenous Access - Establish IV/IO access for fluid and medication administration.
- Fluid Resuscitation - Administer isotonic crystalloids (e.g., normal saline or lactated Ringer's solution) to optimize preload.
Specific Interventions
- Hypovolemic Shock: Focuses on fluid replacement to restore intravascular volume.
- Cardiogenic Shock: Use of inotropes to enhance cardiac contractility and reduce afterload.
- Obstructive Shock: Relief of the obstruction causing the shock (e.g., needle decompression for tension pneumothorax).
- Distributive Shock: Administration of vasopressors to counteract vasodilation (e.g., norepinephrine for septic shock).
Advanced Hemodynamic Monitoring
- Continuous monitoring of ECG, blood pressure, and oxygen saturation (SaO2).
- Use of near-infrared spectroscopy (NIRS) to monitor trends in central venous oxygen saturation (ScvO2).
- Invasive monitoring (e.g., central venous pressure - CVP) as indicated based on the shock type and severity.
Specific Conditions
- Sepsis: Early administration of broad-spectrum antibiotics along with fluid resuscitation and vasopressors.
- Cardiogenic Shock: Mechanical circulatory support (e.g., intra-aortic balloon pump or extracorporeal membrane oxygenation - ECMO) may be considered for patients with severe ventricular dysfunction.
- Early recognition and goal-directed therapy are crucial.
- Reassessment and adjustment of therapy based on the evolving clinical status.
- Use of advanced therapies like ECMO in cases of refractory shock.