Antiarrhythmic Drugs
Antiarrhythmic Drugs
Learning Objectives
- Describe the basic strategies in treating different arrhythmias based on their origin
- Explain how channel blockers work
- Compare and contrast the four major antiarrhythmic drug classes in their mechanisms of action and indications: Class I and III; Class II, IV, and V
- List prototype drugs, clinical uses, side effects, and toxicities in the four major AA classes
- List other AA drugs and describe mechanisms of action, clinical uses, side effects, and toxicities
Antiarrhythmic Drug Classes

Class I: Sodium Channel Blockers (NCB)
Prototype Drugs: Quinidine, Procainamide, Disopyramide, Lidocaine, Mexiletine, Propafenone, Flecainide
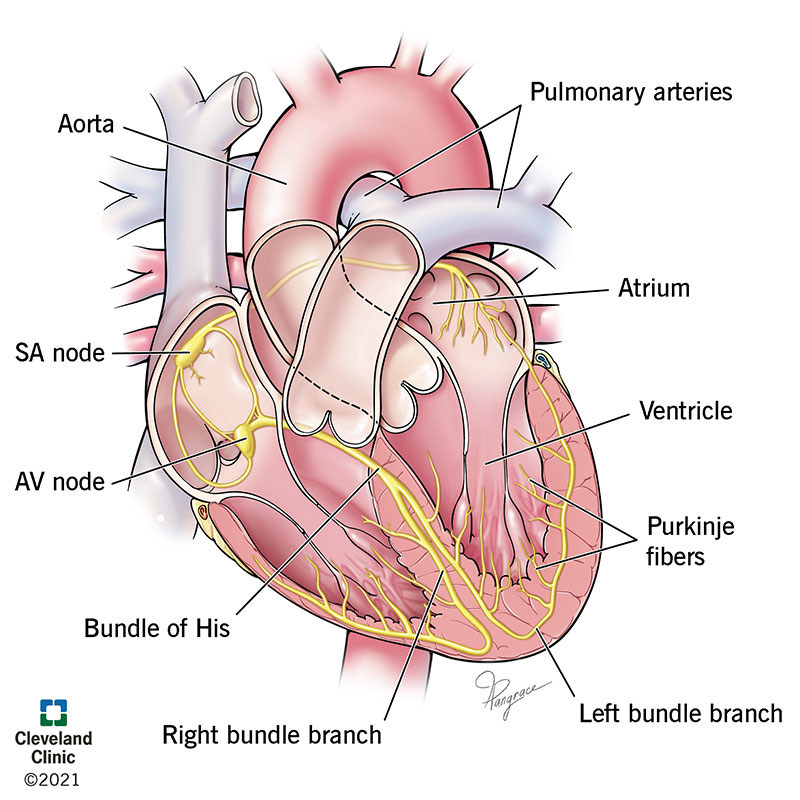
Mechanism of Action: Block sodium channels, which decreases the rate of rise of phase 0 of the action potential in cardiac cells, thereby slowing conduction in the heart.
Indications: Used for various types of arrhythmias depending on the subclass (IA, IB, IC). Class IA (e.g., Quinidine) for atrial and ventricular arrhythmias. Class IB (e.g., Lidocaine) primarily for ventricular arrhythmias. Class IC (e.g., Flecainide) for severe ventricular arrhythmias.
Side Effects and Toxicities: Could include arrhythmias (proarrhythmic effects), dizziness, and visual disturbances. Quinidine may cause headache and ringing in the ears. Procainamide can induce a lupus-like syndrome.
Class II: Beta-Blockers (BB)
Prototype Drugs: Propranolol, Esmolol, Metoprolol
Mechanism of Action: Reduce the effects of adrenaline and other stress hormones on the heart by blocking beta-adrenergic receptors, decreasing heart rate and the force of contraction.
Indications: Supraventricular tachycardia (SVT), ventricular rate control for atrial fibrillation (A-fib) and atrial flutter (A-flutter).
Side Effects and Toxicities: Impotence, exacerbation of chronic obstructive pulmonary disease (COPD) or asthma, cardiovascular effects (bradycardia, AV block, heart failure), and central nervous system effects (sedation, sleep alterations). Metoprolol may cause dyslipidemia, and propranolol can increase vasospasm in vasospastic angina.
Class III: Potassium Channel Blockers (KCB)
Prototype Drugs: Amiodarone, Ibutilide, Dofetilide, Sotalol
Mechanism of Action: Prolongs the action potential duration by blocking potassium channels, thus extending the refractory period and preventing reentrant arrhythmias.
Indications: Used for refractory atrial and ventricular arrhythmias.
Side Effects and Toxicities: Amiodarone has long half-life and potential toxicities, including pulmonary fibrosis, liver toxicity, thyroid dysfunction, and blue-gray skin discoloration.
Class IV: Calcium Channel Blockers (CCB)
Prototype Drugs: Verapamil, Diltiazem
Mechanism of Action: Reduce the influx of calcium ions during the plateau phase (phase 2) of the action potential, decreasing the heart's contractility and conduction velocity.
Indications: Decrease AV nodal conduction and control the ventricular rate in SVT, atrial fibrillation, and flutter.
Side Effects and Toxicities: Constipation, flushing, edema, heart failure, AV block, and reduced sinoatrial (SA) node activity.

Class V: Miscellaneous Agents
Prototype Drugs: Adenosine, Digoxin, Magnesium sulfate
Adenosine: Mechanism of Action: Increases potassium efflux and diminishes calcium influx, leading to hyperpolarization of AV nodal tissue. It's the drug of choice for certain forms of SVT.
Side Effects: Flushing, hypotension, chest pain, sense of impending doom, and bronchospasm.
Digoxin: Mechanism of Action: Inhibits Na+/K+ ATPase leading to an increase in intracellular calcium, resulting in reduced heart rate and increased contractility.
Side Effects: Nausea, vomiting, diarrhea, blurriness, arrhythmias, AV block, and hyperkalemia.

Rate vs. Rhythm Control

- Rate Control: Focuses on slowing down AV conduction to control ventricular rate. Drugs include BB, CCB, and Digoxin.
- Rhythm Control: Aims to fix the abnormal rhythm or fry structural abnormalities to correct reentrant circuits. Drugs include NCB and KCB.
Summary of Cardiac vs. Arterial Selectivity in CCB
- Dihydropyridines: More effect on vasodilation, less effect on heart function (e.g., Nifedipine).
- Non-Dihydropyridines: More effect on heart function, less effect on vasodilation (e.g., Verapamil, Diltiazem).
Adverse Effects

- Adenosine: Flushing, hypotension, coronary steal, and 'sense of impending doom.'
- Amiodarone: Pulmonary fibrosis, liver toxicity, thyroid dysfunction, blue-gray skin.
- Beta-Blockers: Exacerbation of asthma/COPD, sedation, dyslipidemia.
- Digoxin: Nausea, vomiting, diarrhea, blurry yellow vision, arrhythmias.