Coronary Arteries and Blood Flow
Coronary Arteries and Blood Flow

Coronary Artery Anatomy
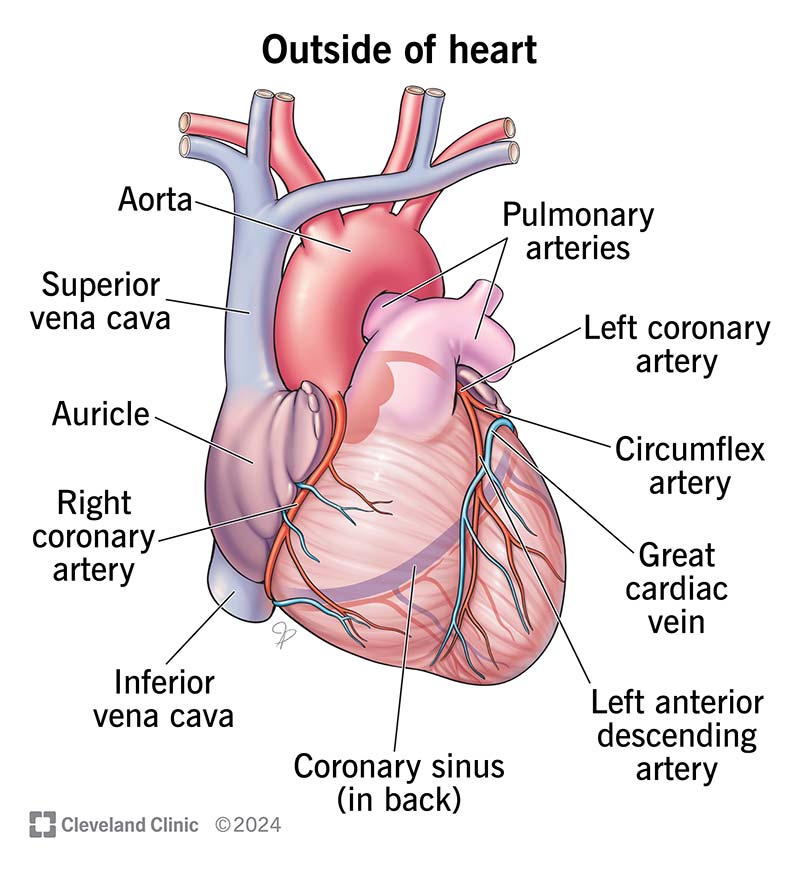
The coronary circulation system comprises the arteries and veins that supply blood to and from the heart muscle (myocardium). The key components include:
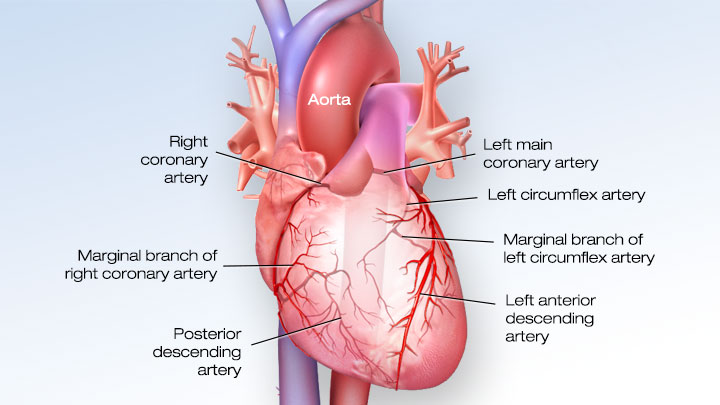
Major Coronary Arteries
- Left Coronary Artery (LCA): Divides into two primary branches:
- Left Anterior Descending Artery (LAD): Supplies the front and bottom of the left side of the heart and the front of the septum.
- Circumflex Artery (LCX): Supplies the left atrium side and the back of the left ventricle.
- Right Coronary Artery (RCA): Supplies the right atrium, right ventricle, bottom portion of both ventricles, and back of the septum. It also gives rise to the right (acute) marginal artery and the posterior descending artery (PDA) in most individuals.
- Additional branches include the diagonal arteries from the LAD, and the left (obtuse) marginal artery from the LCX.

Coronary Veins
- Great Cardiac Vein: Runs alongside the LAD, collecting blood from the left anterior descending territory.
- Small Cardiac Vein: Collects blood from the right margin of the heart.
- Middle Cardiac Vein: Runs in the posterior interventricular sulcus.
- Coronary Sinus: Collects most of the venous blood from the heart and drains into the right atrium.
Unique Aspects of Coronary Blood Flow
Three unique features differentiate coronary circulation from the rest of the body's vascular system:

1. Coronary Arteries Fill During Diastole
- Unlike other vascular beds, coronary arteries fill primarily during the diastolic phase of the cardiac cycle.
- The aorta stores energy in its elastic walls during systole, which is released during diastole, aiding in coronary perfusion.
- Diastolic blood pressure is a key determinant of coronary blood flow.
- Pathologies like aortic regurgitation can lead to impaired coronary perfusion.

2. High Oxygen Extraction
- The myocardium extracts about 70% of the oxygen from the blood at rest, which is significantly higher than in other tissues like skeletal muscle (20-40%).
- Coronary veins such as the great cardiac vein have some of the lowest venous oxygen concentrations in the body.
- Due to high basal oxygen extraction, the heart's ability to increase oxygen extraction during stress is limited, relying instead on increased blood flow to meet higher oxygen demands.

3. Metabolic Regulation Over Neural Control
- Coronary blood flow is primarily regulated by metabolic activity of the myocardium rather than autonomic nervous system (ANS) control.
- Vasodilation: Driven by local metabolites including adenosine (a byproduct of ATP metabolism), nitric oxide (NO), endothelial-dependent vasodilators, prostacyclin, and endothelial-derived hyperpolarizing factor (EDHF).
- Vasoconstriction: Includes agents like endothelin-1 and stimuli of the sympathetic nervous system (SNS), although the SNS effect is less pronounced than metabolic factors.

Flow Across Stenosis
- The hemodynamic significance of a coronary artery stenosis depends on its length and the degree of vessel narrowing.
- Despite continuous flow across the stenosis, flow velocity increases at the stenosis site, while pressure decreases.
- Pressure may increase before the stenosis as an adaptive response.
- Poiseuille’s Law and Ohm's Law apply to blood flow dynamics through stenosed arteries:
- Poiseuille’s Law: Relates to flow resistance in the vessel.
- Ohm's Law: ΔP = Q x R (Pressure gradient = Flow rate x Resistance).
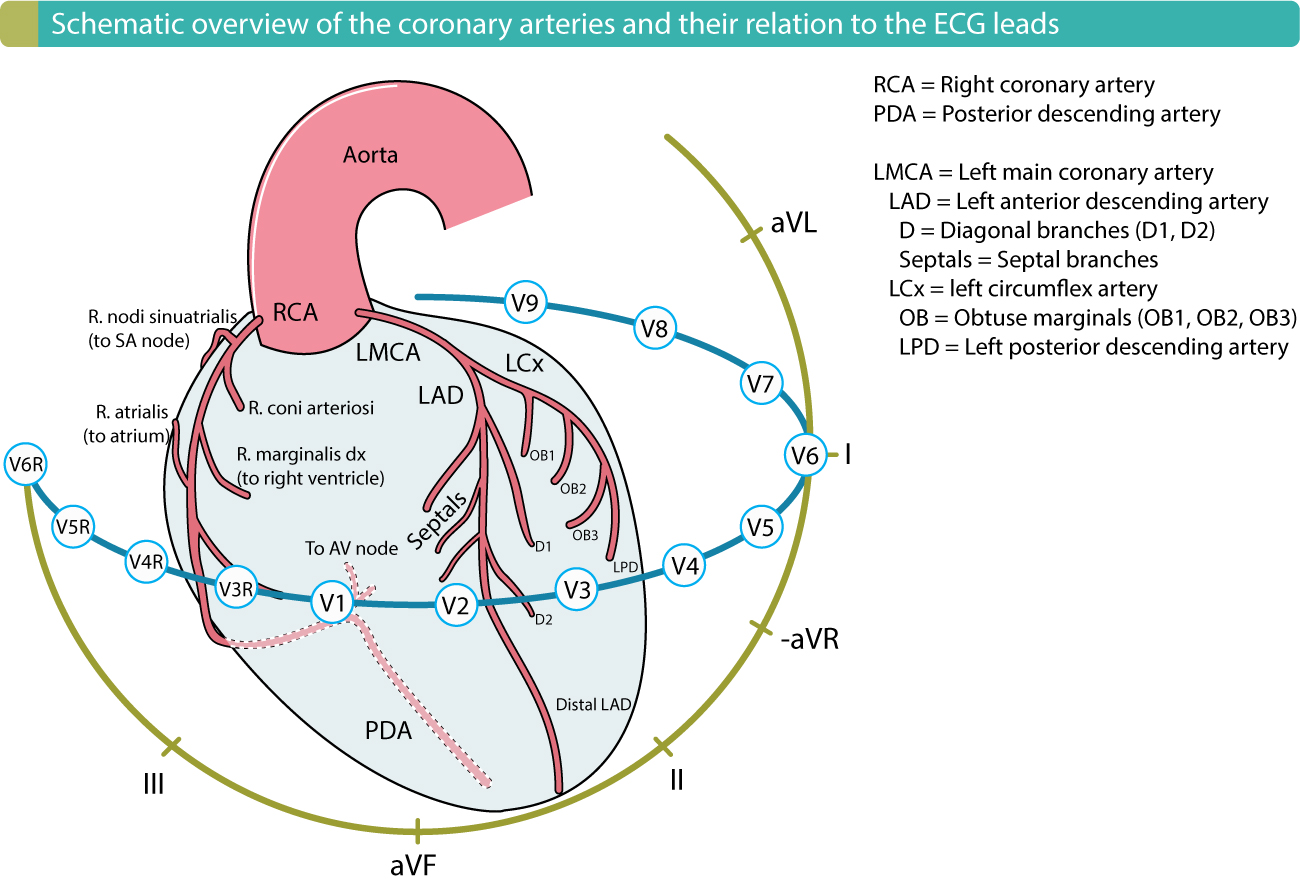
Clinical Correlation: Localizing Myocardial Infarctions
Table 1: Localization of Ischemic Area in ST Elevation Myocardial Infarction (STEMI/STE-ACS)
- Anteroseptal (LAD): Leads V1-V2.
- Anteroapical (distal LAD): Leads V3-V4.
- Anterolateral (LAD or LCX): Leads V5-V6.
- Lateral (LCX): Leads I, aVL.
- Inferior (RCA): Leads II, III, aVF.
- Posterior (PDA): Leads V7-V9, with ST depression in V1-V3 and tall R waves.
Understanding these unique aspects of coronary blood flow and anatomy is crucial for diagnosing and managing ischemic heart disease.