CV Effects of the Autonomic Nervous System
CV Effects of the Autonomic Nervous System
Lecture Objectives:
- Describe how direct muscarinic agonists and sheer stress cause arterial dilation through endothelial nitric oxide (NO)
- Compare and contrast CV effects of direct/indirect cholinomimetics and muscarinic/ganglionic blockers
- Explain CV effects and therapeutic uses of atropine, the prototype muscarinic blocker
- Define the predominant tone and describe how ganglionic blockers reverse the tone and block further reflexes
Direct Muscarinic Agonists and Sheer Stress: Arterial Dilation Through Endothelial Nitric Oxide (NO)
Direct Muscarinic Agonists: These stimulate muscarinic receptors on endothelial cells, leading to the activation of endothelial nitric oxide synthase (eNOS). eNOS converts L-arginine to nitric oxide (NO). NO then diffuses into the smooth muscle of the blood vessel wall, where it activates guanylate cyclase, increasing cGMP levels and causing vasodilation.
Sheer Stress: The physical force of blood flow exerts pressure on the endothelial cells. This mechanical force also stimulates eNOS to produce NO, leading to vasodilation in a manner similar to muscarinic receptor activation.
Comparison: CV Effects of Cholinomimetics and Blockers
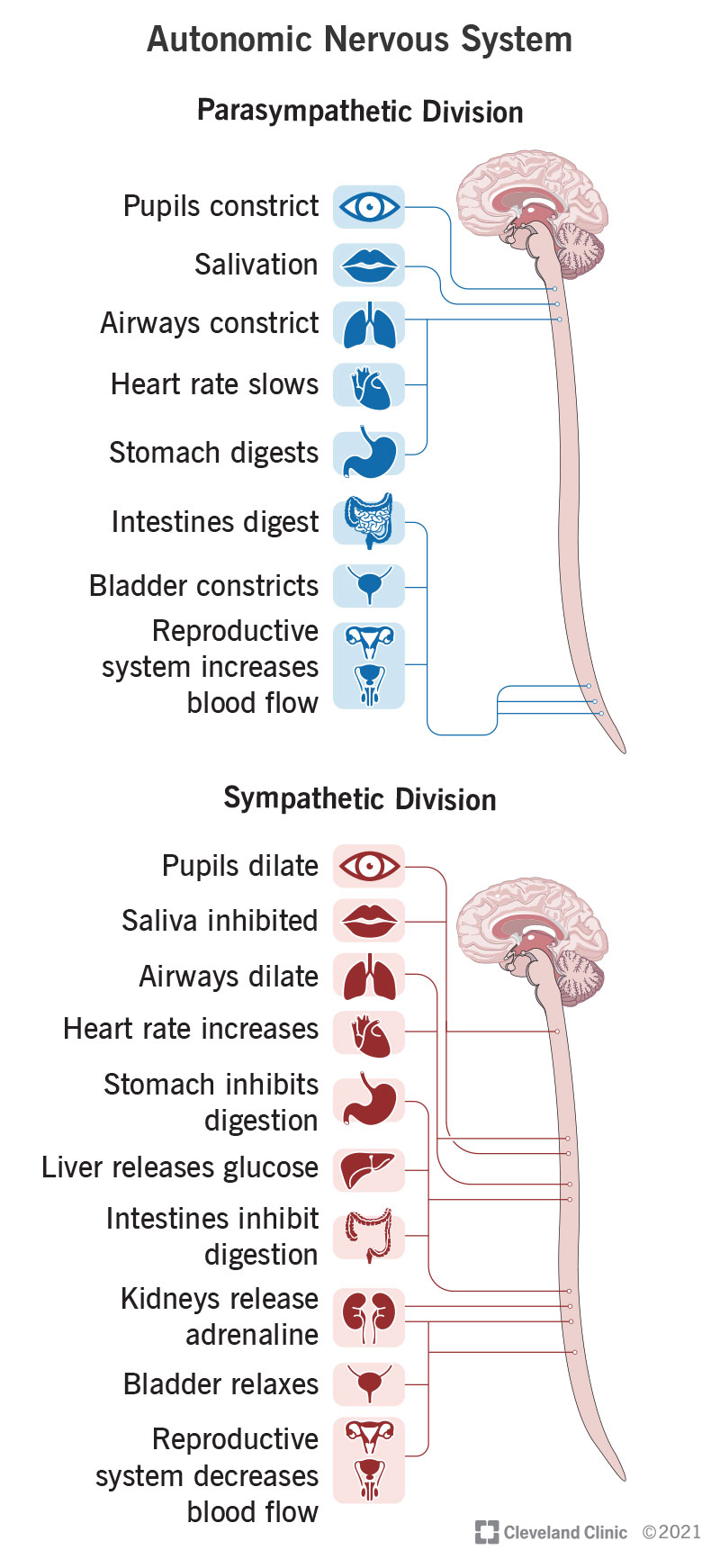
Direct Cholinomimetics (Muscarinic Agonists): These mimic the action of acetylcholine at muscarinic receptors, leading to decreased heart rate (bradycardia), vasodilation, and decreased blood pressure.
Indirect Cholinomimetics: These inhibit acetylcholinesterase, increasing acetylcholine levels, which can enhance both muscarinic and nicotinic effects, causing bradycardia, hypotension, and potential increase in skeletal muscle contraction.
Muscarinic Blockers (e.g., Atropine): Block the action of acetylcholine at muscarinic receptors, leading to increased heart rate (tachycardia), decreased secretions, and potential bronchodilation.
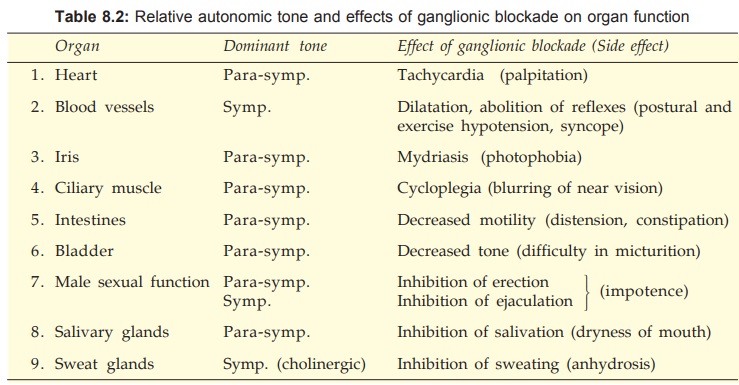
Ganglionic Blockers: These block nicotinic receptors at autonomic ganglia, reducing both sympathetic and parasympathetic outflow. This can cause unpredictable CV effects, including hypotension (due to loss of sympathetic tone) and tachycardia (due to loss of parasympathetic tone).
CV Effects and Therapeutic Uses of Atropine
CV Effects: Atropine blocks muscarinic receptors, leading to increased heart rate (tachycardia) and reduced vagal tone on the heart. It can also reduce secretions and cause mydriasis.
Therapeutic Uses: Atropine is used to treat bradycardia, as a pre-anesthetic to reduce secretions, and to manage organophosphate poisoning (which causes excessive cholinergic activity).
Predominant Tone and Ganglionic Blockers
Predominant Tone: Refers to the dominant autonomic influence on a particular organ system at rest. For example, the heart is predominantly under parasympathetic (vagal) tone, while blood vessels are under sympathetic tone.
Ganglionic Blockers: These drugs block both sympathetic and parasympathetic ganglia. By doing so, they reverse the predominant tone (e.g., causing tachycardia by removing vagal influence on the heart) and prevent further reflexes (e.g., baroreceptor reflexes), leading to effects such as orthostatic hypotension.
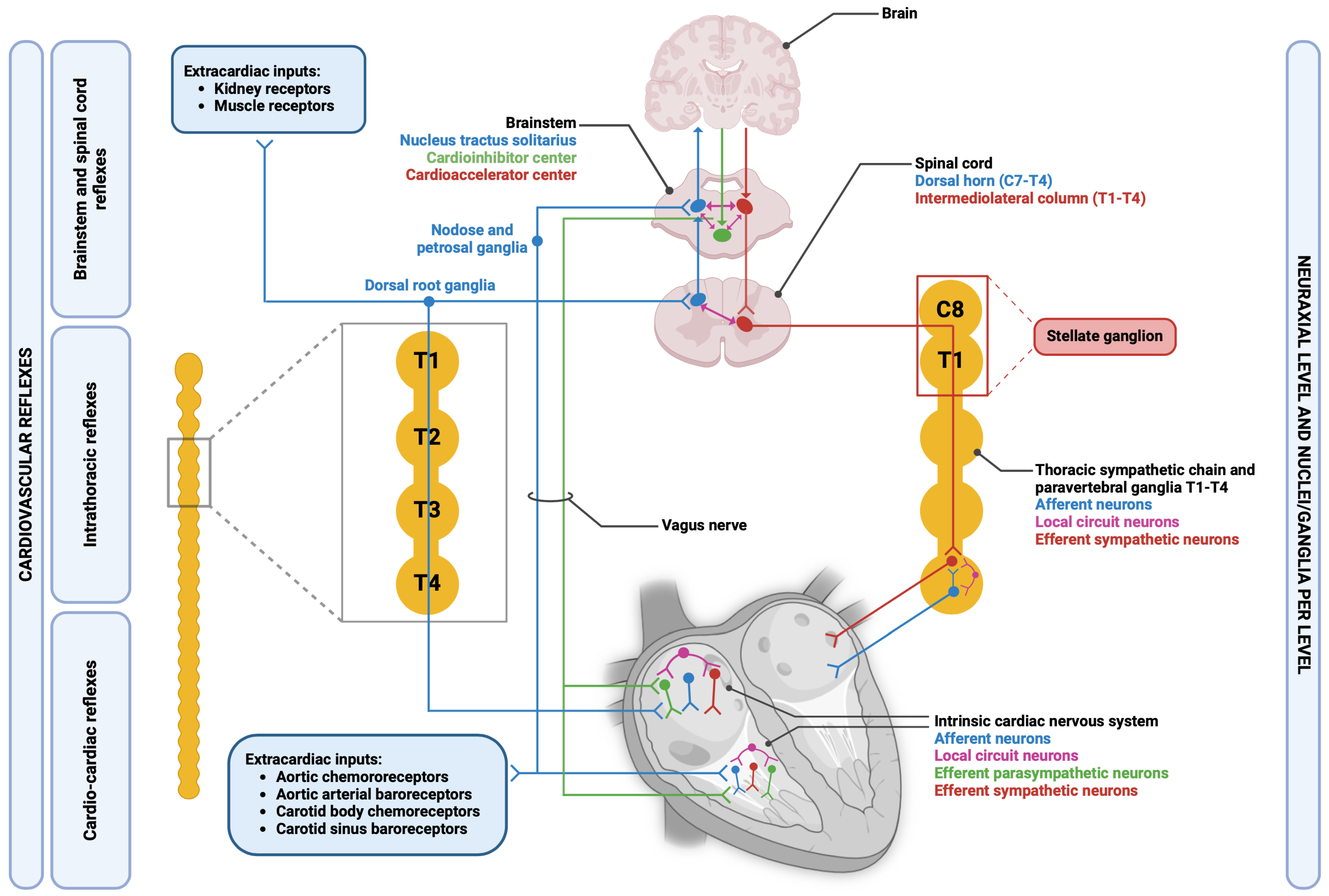
CV Parasympathetic Nervous System (PNS) Innervation and Receptor Subtypes
Innervation of Blood Vessels and Heart: - Arteries and Arterioles: α1 receptors cause vasoconstriction in skin and splanchnic areas, while β2 receptors induce vasodilation in skeletal muscle arteries. - Veins and Venules: α1 receptors cause vasoconstriction. - Heart: Predominantly M2 receptors located at the nodes (SA and AV nodes) with less influence on ventricular myocardium. - Capillaries: Not innervated.
Sympathetic Innervation: Primarily affects arteries, veins, nodes, and ventricles through α1 & β1 receptors.
Parasympathetic (PS) Innervation: Mainly limited to nodes (controlling heart rate) via M2 receptors with non-innervated endothelial M3 receptors.

Mechanisms and Effects of Cholinergic Agonists
Direct Muscarinic Agonists and Sheer Stress: - Mechanism: Direct muscarinic agonists activate M3 receptors on endothelial cells leading to nitric oxide (NO) synthesis. NO then diffuses into smooth muscle cells, activating guanylyl cyclase, increasing cGMP levels, and promoting vasodilation. - Pathway: M3 receptor activation → NO → cGMP → Vasodilation of smooth muscle. - Sheer Stress: Increased blood flow or shear stress can also induce NO production through a similar pathway.
Cholinomimetic Effects on Cardiovascular System: - Low-dose ACh IV: Primarily causes vasodilation by acting on M3 receptors on endothelial cells, reducing peripheral resistance and blood pressure, often accompanied by reflex tachycardia. - High-dose ACh IV: Prominent effects on the heart, leading to bradycardia by decreasing cAMP and activating K+ channels at the SA and AV nodes, thus reducing heart rate and conduction velocity.
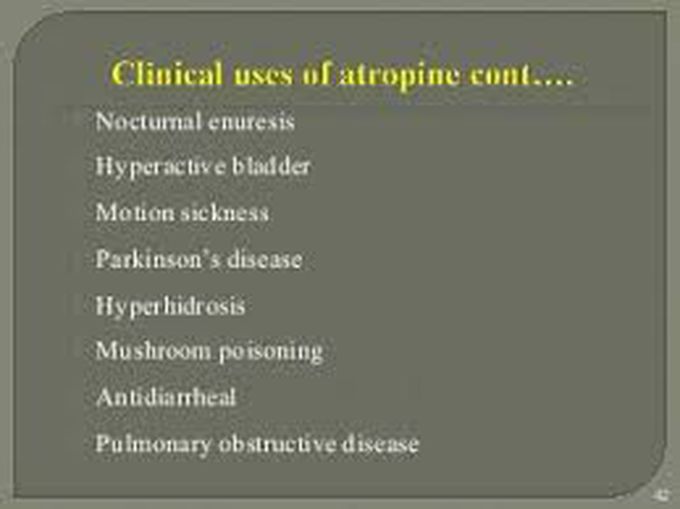
Therapeutic Uses and Effects of Atropine
Atropine (Prototype Muscarinic Blocker): - CV Effects: Increases heart rate by blocking M2 receptors in the heart. No significant effect on blood pressure due to lack of parasympathetic innervation in blood vessels. - Therapeutic Applications: Used to treat bradycardia, reduce secretions during surgery, and as an antidote for organophosphate poisoning.

Ganglionic Blockers and Predominant Tone
Predominant Tone: - Ganglionic Blockers: Affect both sympathetic and parasympathetic outputs at the ganglionic level. Their effects are determined by the predominant tone of the effector organ. - Reversal of Tone: Ganglionic blockers reverse the predominant tone, blocking further parasympathetic or sympathetic reflexes, such as blunting the baroreceptor reflex.
Functional Roles of Nicotinic AChR: - Ganglia: Drugs affecting nicotinic ACh receptors at the ganglionic level will have broad autonomic effects, altering both parasympathetic and sympathetic activities. - Neuromuscular Junction (NMJ): NMJ blockers serve as muscle relaxants during anesthesia. - CNS: Nicotine’s addictive properties stem from its CNS-nicotinic receptor interactions.
Summary of CV ANS Effects - Parasympathetic: Reduces heart rate (HR) through M2 receptors, with negligible direct effects on blood vessels. - Sympathetic: Utilizes α1 receptors for vasoconstriction, β2 for vasodilation in skeletal muscle, and β1 for increasing HR and contractility.
Adverse Reactions and Clinical Uses of Ganglionic Blockers
Adverse Reactions: - Mild: Mydriasis, dry mouth, urinary hesitancy, constipation. - Severe: Postural hypotension, anginal pain, CNS effects like mania and seizures with mecamylamine.
Clinical Uses: - Hypertension: Previously used trimethaphan for hypertension management, now largely replaced by vasodilators. - Autonomic Hyperreflexia: Treated with mecamylamine in cases of spinal cord injury.
Key Pharmacology Rule: Blockers can only inhibit existing or future endogenous activities; they cannot block what is not present.