Diseases of the Pericardium
Diseases of the Pericardium
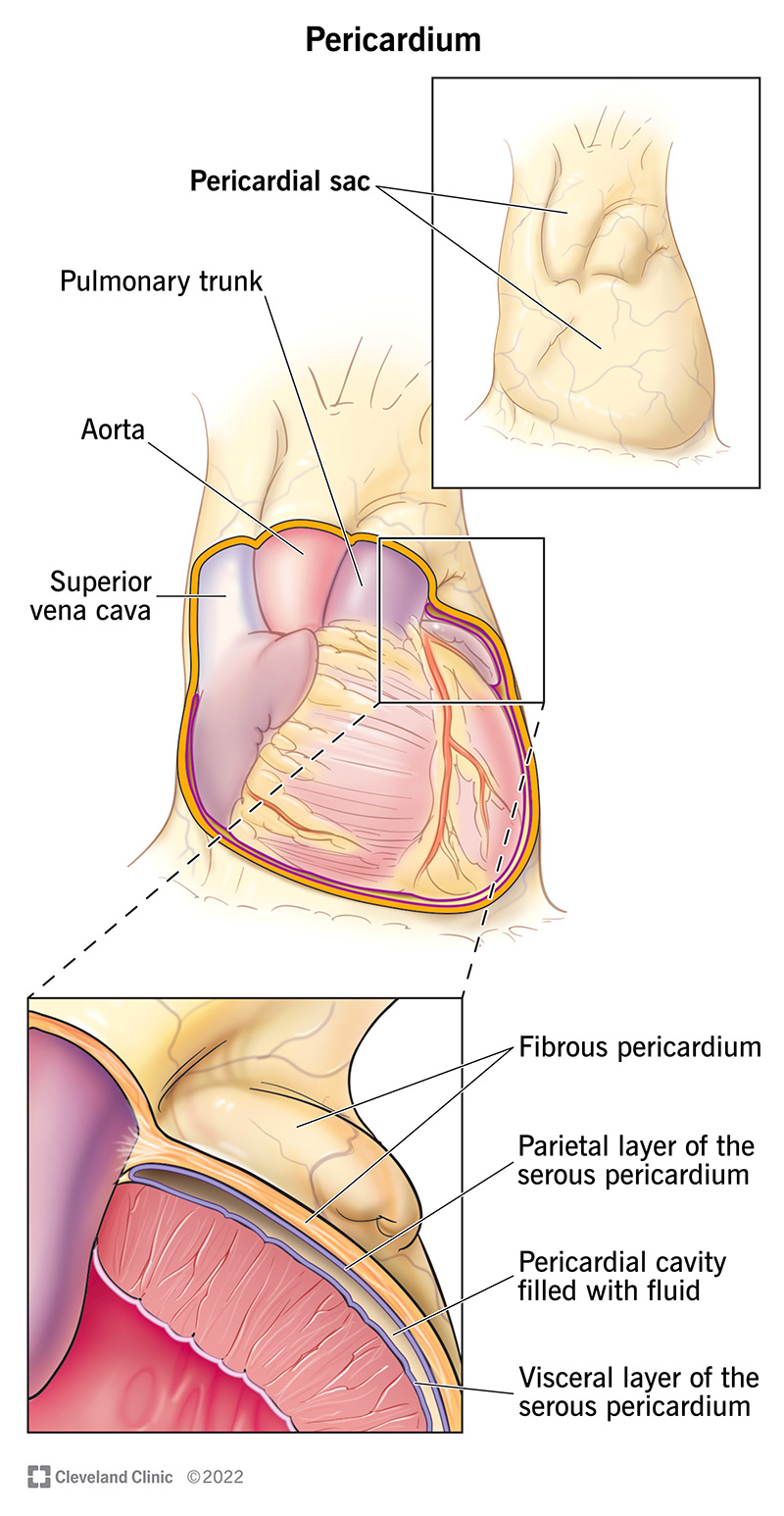
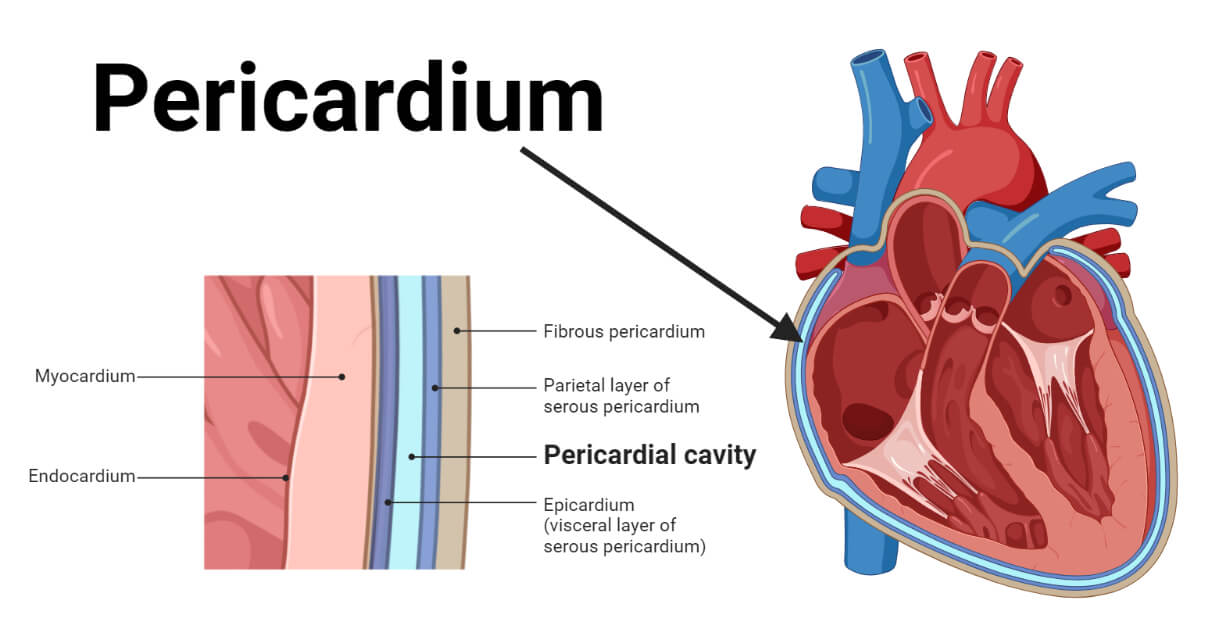
Pericardial Anatomy
The pericardium is a two-layered sac that encircles the heart. It consists of:
- Fibrous pericardium: The outer (parietal) fibrous layer.
- Serous pericardium: The inner (visceral) serosal layer, which has two subdivisions: the parietal pericardium and the visceral pericardium.
A thin layer of fluid, called pericardial fluid, separates the parietal and visceral layers of the pericardium.
Pericardial Function
The pericardium serves several important functions:
- Fixes the heart within the mediastinum: It keeps the heart positioned within the chest cavity.
- Prevents extreme dilation of the heart: It restricts excessive expansion of the heart.
- Barrier to infection: It prevents the spread of infection from adjacent structures.
Etiology of Acute Pericarditis
Acute pericarditis can be caused by various factors. These can be broadly categorized into infectious and noninfectious causes.
Infectious Causes
- Viral: Common viruses include echovirus, coxsackievirus group B, influenza, varicella, mumps, hepatitis B, and mononucleosis.
- Bacterial: Often seen in immunocompromised patients or those with chest trauma or surgery. Common bacteria include pneumococci and staphylococci.
- Tuberculous: Typically occurs in immunosuppressed patients through reactivation, direct spread from the lungs, or hematogenous dissemination.
Noninfectious Causes
- Idiopathic: No specific cause identified.
- Post MI (Myocardial Infarction): Can be acute or delayed (Dressler syndrome).
- Uremic: Often seen in untreated chronic renal failure.
- Neoplastic: Metastatic spread or local invasion by tumors.
- Radiation induced: Post-radiotherapy.
- Autoimmune: Diseases like systemic lupus erythematous, rheumatoid arthritis, and systemic sclerosis.
- Drug-induced: Due to medications.
Clinical Features of Acute Pericarditis
Acute pericarditis is characterized by:
- Pleuritic chest pain: Sharp, positional pain that is worse with inspiration or coughing.
- Fever
- Friction rub: Can be intermittent.

Pathogenesis of Acute Pericarditis
The pathogenesis involves three stages, similar to other inflammatory processes:
- Vasodilation: Initial response causes increased blood flow.
- Increased vascular permeability: Fluid and proteins leak into tissues.
- Exudation: Accumulation of inflammatory cells and proteins.
The pathologic appearances include:
- Serous pericarditis: An early response with thin fluid, common to all types.
- Serofibrinous pericarditis: The most common form, with fusion of the visceral and parietal pericardium.
- Suppurative (purulent) pericarditis: Usually seen with bacterial infections.
- Hemorrhagic pericarditis: Commonly associated with tuberculosis or malignancy.
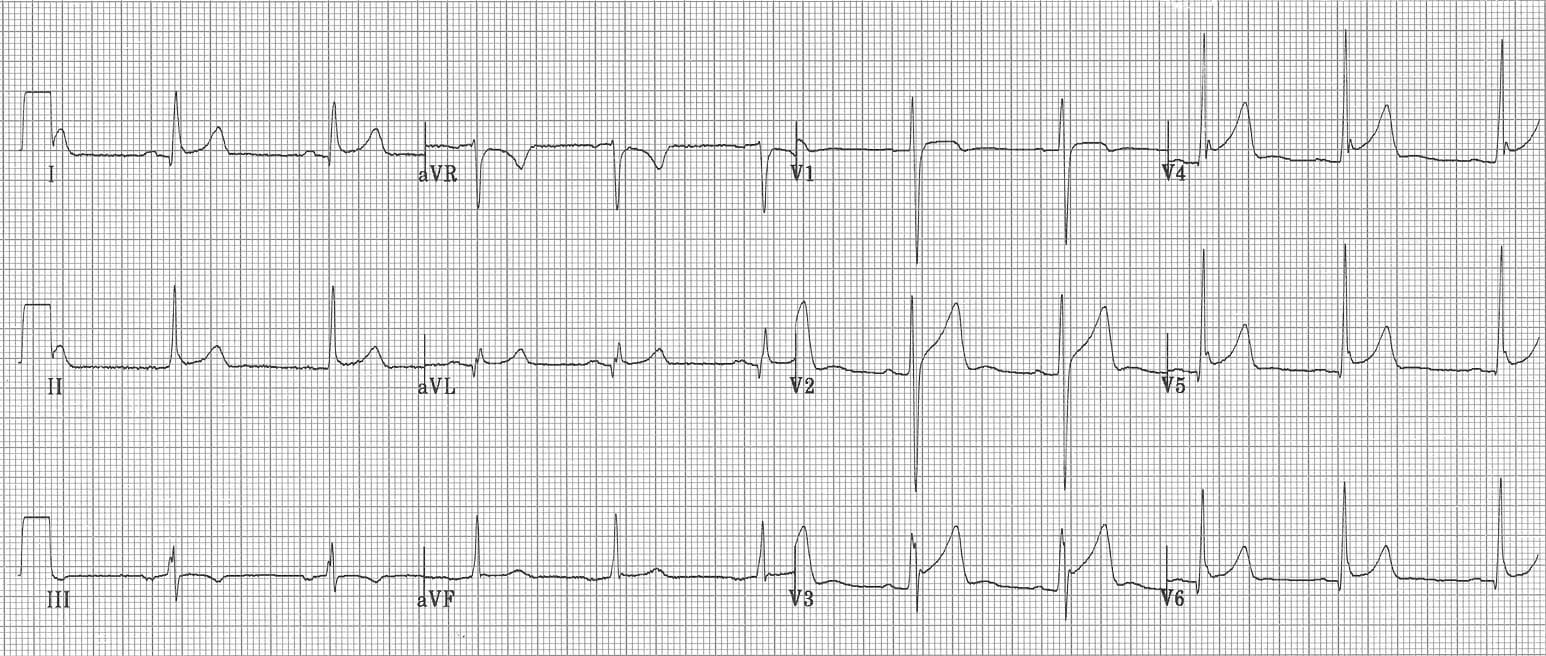
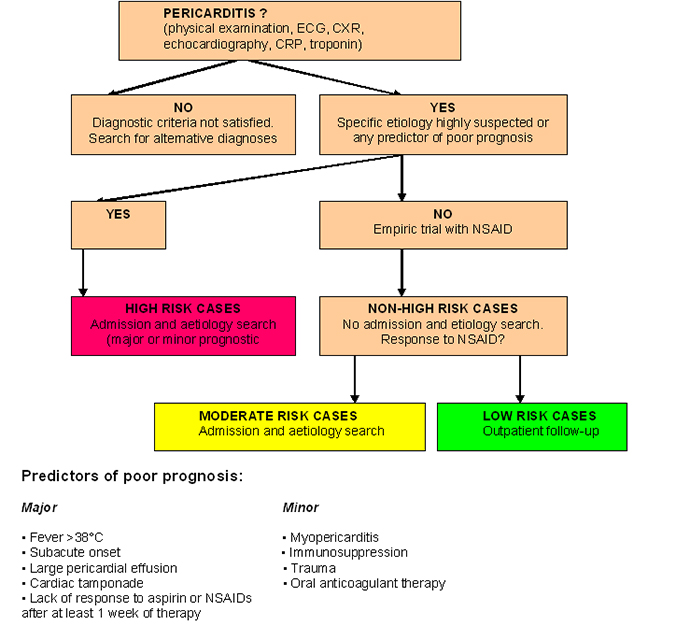
Diagnosis of Acute Pericarditis
Diagnosis is primarily through:
- ECG Changes: Typically shows diffuse ST-segment elevations.
- Echocardiography: Shows thickening of the pericardium and fluid accumulation.
Treatment of Acute Pericarditis
Idiopathic or Viral Pericarditis
- Generally self-limited, resolving in about 1-3 weeks.
- Pain relief with anti-inflammatory drugs such as aspirin, ibuprofen, or NSAIDs.
- Colchicine may be added.
- Steroids for severe or recurrent cases.
Purulent Pericarditis
- Requires more aggressive treatment with drainage and IV antibiotics.
Uremic Pericarditis
- Treated with hemodialysis.
Pericardial Effusion
The pericardial space normally contains 15-50 mL of fluid. Symptoms develop when there is compression of the heart due to increased fluid volume.
Clinical Features and Diagnosis
- Muffled heart sounds
- Electrical alternans: Variation of the QRS complex.
- Echocardiography: Key diagnostic tool and useful for pericardiocentesis.

Cardiac Tamponade
This is a high-pressure accumulation of pericardial fluid leading to diastolic compression of all cardiac chambers, limiting filling, and resulting in decreased stroke volume and cardiac output.
Clinical Features
- Beck's Triad: Jugular venous distention, systemic hypotension, and muffled heart sounds.
- Sinus tachycardia
- Pulsus paradoxus: A ≥10 mmHg decrease in systolic BP with inspiration.
Causes
- Post-viral, neoplastic, uremic, acute hemorrhage (trauma or post-thoracic surgery).
Diagnosis and Treatment
- Diagnosis through clinical assessment, echocardiography, and cardiac catheterization.
- Pericardiocentesis: Removal of the high-pressure fluid as the primary intervention.

Constrictive Pericarditis
This condition develops over months to years and involves the formation of a fibrous scar, potentially with calcification.
Pathology
- Inhibits normal filling: Venous pressure rises, leading to signs of right heart failure and decreased cardiac output.
- Kussmaul sign: Jugular veins more distended during inspiration.
- Echo, CT, or MRI: Imaging techniques to assess pericardial thickening and calcification.
- Cardiac catheterization: Shows elevation and equalization of diastolic pressures and the square root sign.
- Surgical pericardiectomy: Removal of the pericardium.