Cardiovascular Effects of the Autonomic Nervous System (ANS)
Cardiovascular Effects of the Autonomic Nervous System (ANS)
Learning Objectives
- Explain how the ANS regulates CV function.
- Describe mechanisms of short-term blood pressure control and explain the role of baroreceptors.
- Explain how prototype sympathomimetics affect blood pressure and heart rate.
Autonomic Nervous System (ANS)
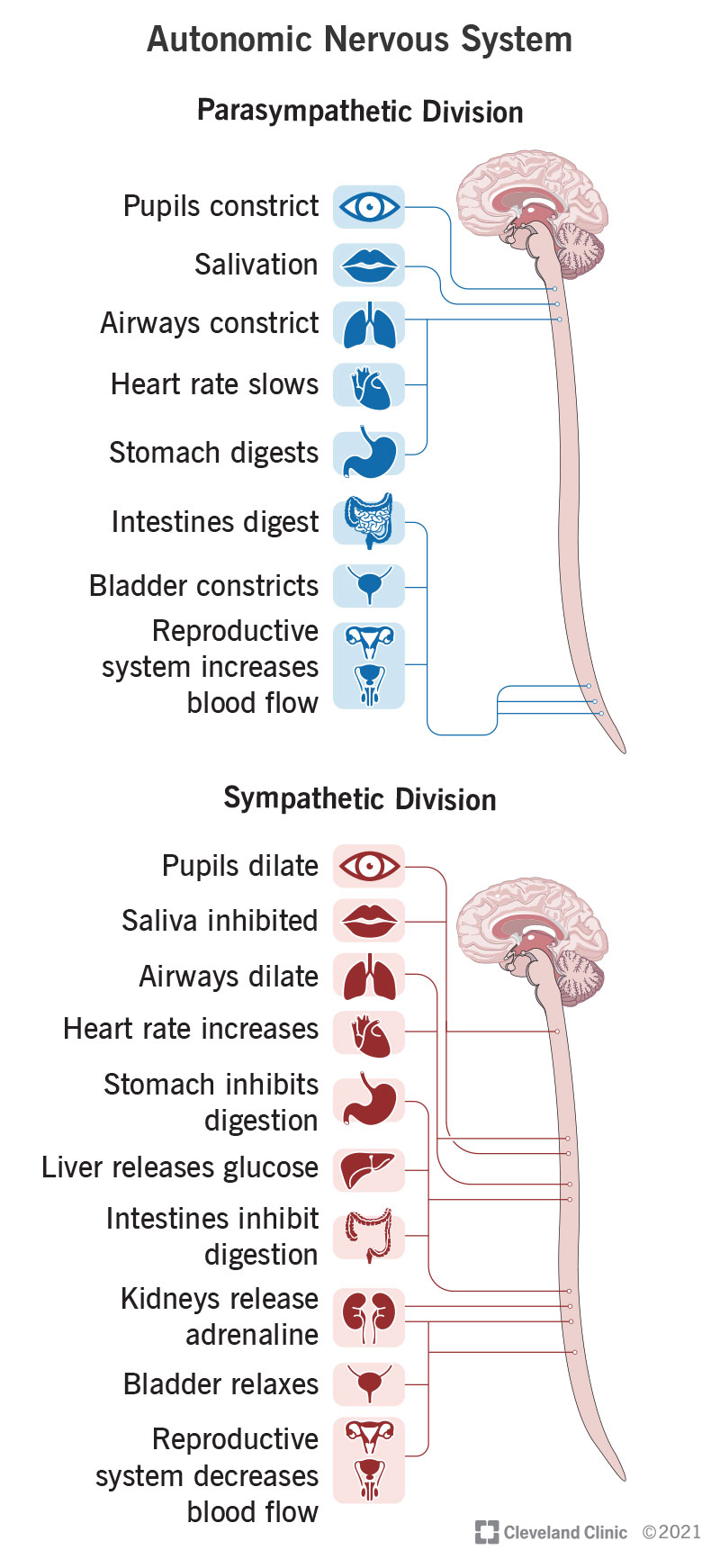
The ANS regulates cardiovascular (CV) function through its two main divisions: the sympathetic and parasympathetic nervous systems, each impacting various organs like the eyes, heart, lungs, and more in different ways.
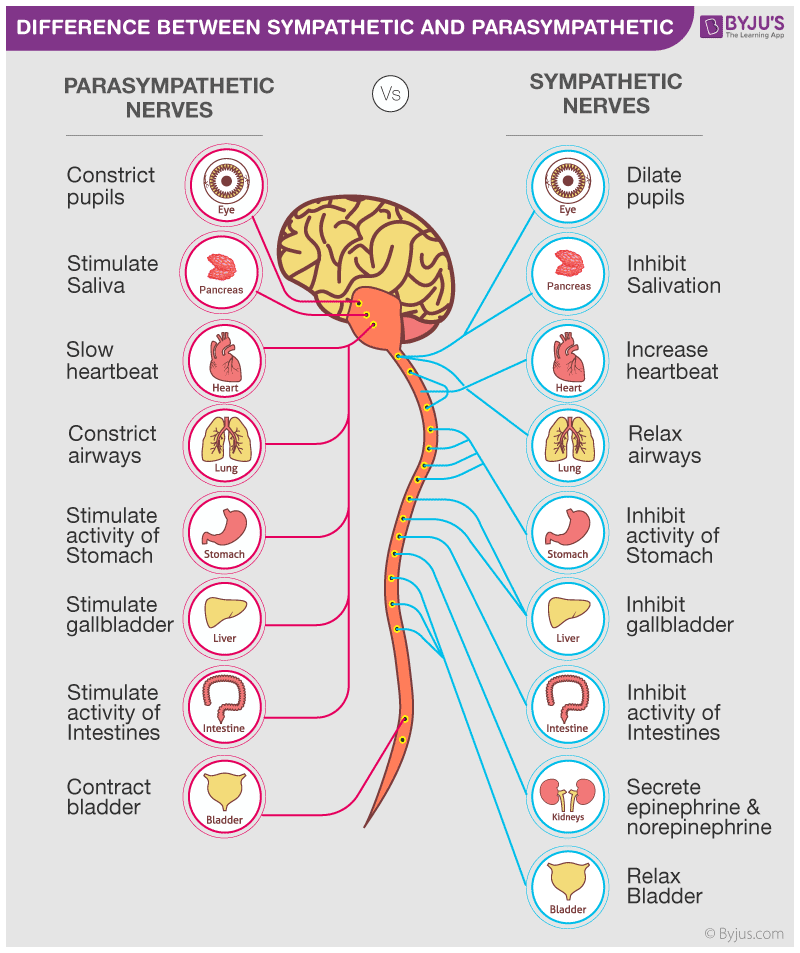
Parasympathetic vs. Sympathetic Comparison
- Parasympathetic System: Constricts pupils, stimulates salivation, slows the heartbeat, constricts bronchi, stimulates digestion, stimulates bile release, and contracts the bladder.
- Sympathetic System: Dilates pupils, inhibits salivation, accelerates heartbeat, dilates bronchi, inhibits digestion, stimulates glucose release, stimulates epinephrine, and norepinephrine release, and relaxes the bladder.
The Sympathetic Nervous System
- Heart: Accelerates heartbeat, increases conduction velocity, and enhances contractility.
- Blood Vessels: Causes generalized vasoconstriction, with exceptions like vasodilation in skeletal muscles.
- Lungs: Dilates bronchi.
- Metabolism: Increases gluconeogenesis, glycogenolysis, and lipolysis.
- Glands and Organs: Promotes sweat secretion and inhibits digestive activity.
:background_color(FFFFFF):format(jpeg)/images/library/13927/Parasympathetic_nervous_system.png)
The Parasympathetic Nervous System
- Heart: Slows heartbeat and reduces conduction velocity.
- Blood Vessels: Promotes vasodilation in specialized tissues.
- Lungs: Constricts bronchi.
- Digestive System: Stimulates activity in the gastrointestinal tract.
- Glands: Promotes secretion in salivary and nasopharyngeal glands.
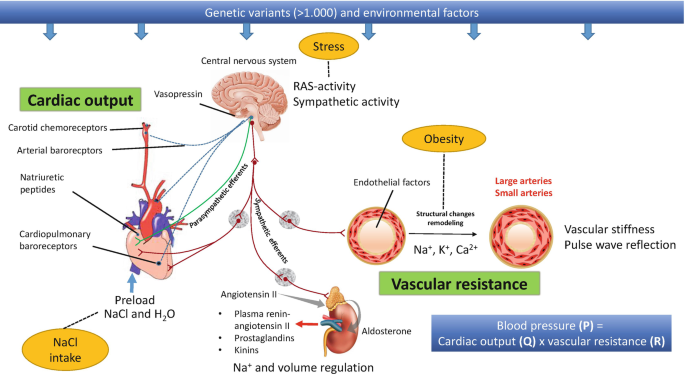
Mechanisms of Blood Pressure Regulation
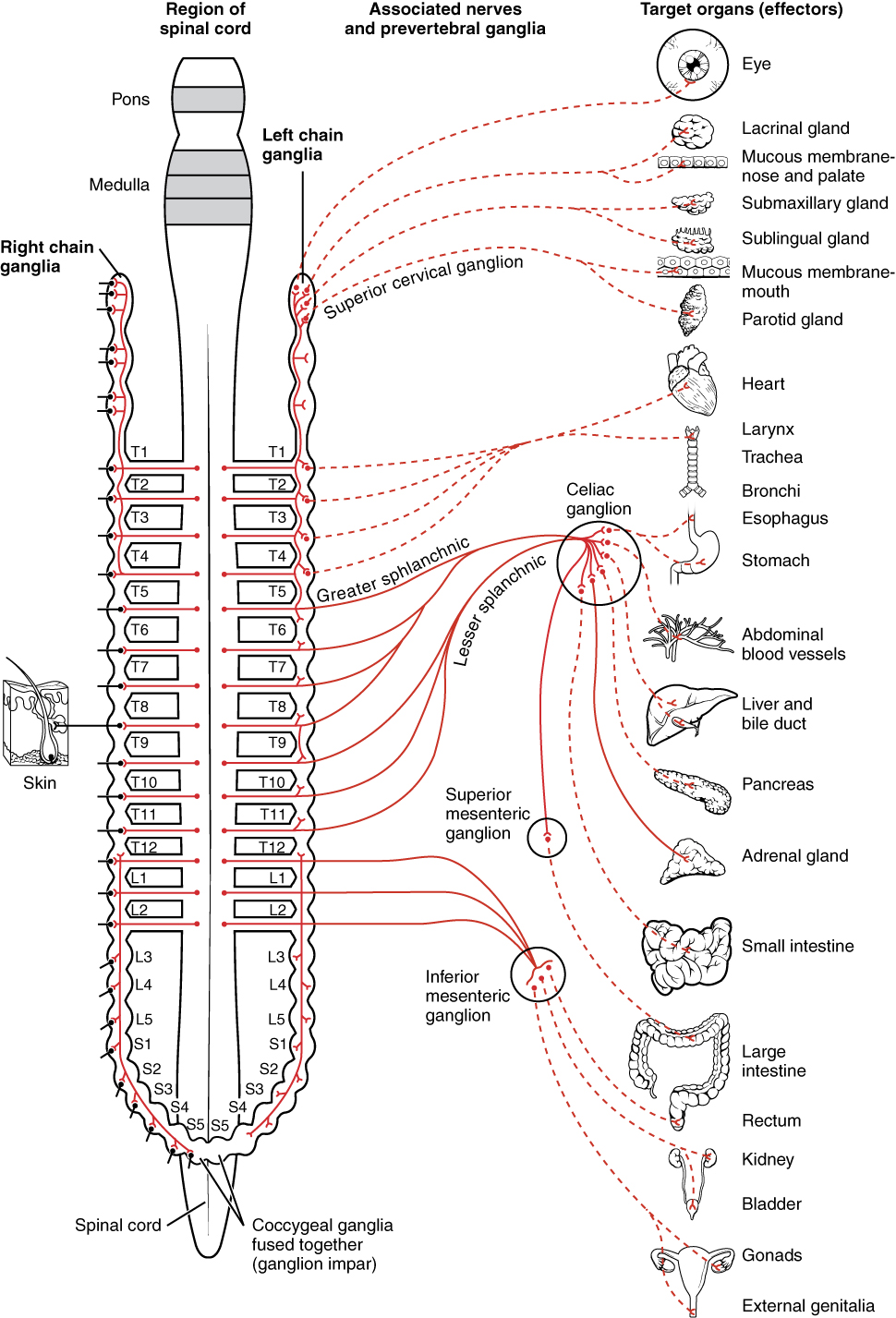
1. Sympathetic Innervation
- Blood Vessels: Arteries and veins are innervated only by the sympathetic system. Increased activity causes vasoconstriction (α1 receptors) in major vascular beds and vasodilation in skeletal muscle arterioles (β2 receptors).
- Heart: Sympathetic nerves enhance heart rate and contractility via β1 receptors. Parasympathetic effects via vagus nerve (M2 receptors) decrease heart rate.
2. Adrenergic Receptor Subtypes and Intracellular Mechanisms
- α1 Receptors: Linked with Gq proteins, increase IP3 and DAG, leading to increased intracellular Ca2+ and vasoconstriction.
- α2 Receptors: Associated with Gi proteins, decrease cAMP, and reduce norepinephrine release.
- β1 Receptors: Stimulatory effects, increase cAMP, enhancing heart rate, contractility, and renin release.
- β2 Receptors: Also increase cAMP, but primarily causing vasodilation and bronchodilation.
3. Baroreceptors
- Located in the carotid sinus and aortic arch, baroreceptors detect changes in arterial pressure. Increased pressure stretches baroreceptors, increasing their firing rate. This activates a negative feedback loop involving the vagus nerve and medulla, reducing sympathetic outflow and increasing parasympathetic activity to decrease blood pressure and heart rate.
- Conversely, decreased pressure lowers baroreceptor firing, increasing sympathetic activity and decreasing parasympathetic output, raising blood pressure and heart rate to normal levels.
Frank-Starling Law
This law states that the stroke volume of the heart increases in response to an increase in the volume of blood filling the heart (end-diastolic volume or EDV). Mechanisms include:
- Increased EDV stretches the ventricular walls, leading to a more forceful contraction.
- Greater stroke volume ultimately generates higher cardiac output.
- Factors influencing this include preload, afterload, and contractility.

Clinical Applications
Sympathomimetics in Cardiac Care:
- Dobutamine/Dopamine: Used in acute heart failure or shock to increase cardiac contractility and reduce afterload through minor β2 effects, though they may cause arrhythmias.
- Norepinephrine (NE): Increases blood pressure primarily through α1-mediated vasoconstriction, also affecting β1 receptors in the heart.
- Phenylephrine: Utilized as a nasal decongestant due to its α1 agonist properties.
- Clonidine: An α2 agonist used to decrease blood pressure through CNS effects.
Adrenergic Drug Effects:
- Epinephrine: Acts on α1, α2, β1, and β2 receptors, causing increased heart rate, contractility, vasoconstriction, and vasodilation.
- Norepinephrine: Influences α1, α2, and β1 receptors, enhancing heart contractility and causing vasoconstriction without β2 actions.
- Isoproterenol: Stimulates β1 and β2 receptors, leading to increased heart rate and contractility with vasodilation.

Hormonal Regulation - RAAS
The Renin-Angiotensin-Aldosterone System (RAAS) significantly influences blood pressure and fluid balance:
- Renin: Released from kidneys in response to low blood pressure or sympathetic activation.
- Angiotensin II: Formed through Angiotensin I conversion by ACE; it elevates blood pressure via vasoconstriction and stimulates aldosterone release.
- Aldosterone: Promotes sodium and water retention, increasing blood volume and preload, thus raising blood pressure.
Key highlights involve the role of AT1 receptors and ACE inhibition in therapeutics.