Cardiovascular Effects of the Autonomic Nervous System (ANS)
Cardiovascular Effects of the Autonomic Nervous System (ANS)

Lecture Objectives
- Describe how direct muscarinic agonists and sheer stress cause arterial dilation through endothelial nitric oxide (NO)
- Compare and contrast CV effects of direct/indirect cholinomimetics and muscarinic/ganglionic blockers
- Explain CV effects and therapeutic uses of atropine, the prototype muscarinic blocker
- Define the predominant tone and describe how ganglionic blockers reverse the tone and block further reflexes

CV PNS Innervation and Receptor Subtypes
Innervation of Blood Vessels
Blood vessels do not have parasympathetic innervation. However, they do possess orphan muscarinic receptors (primarily M3) on endothelial cells. These receptors are not innervated but can respond to circulating muscarinic agonists, causing vasodilation through the nitric oxide (NO) pathway.

Innervation of the Heart
The heart receives both sympathetic and parasympathetic innervation. Sympathetic fibers (primarily using β1 adrenergic receptors) innervate the nodes and ventricles, promoting increased heart rate (HR) and contractility. Parasympathetic fibers (via M2 muscarinic receptors) innervate the nodes, primarily the SA and AV nodes, to decrease HR.

Receptor Subtypes in the Cardiovascular System
- α1 (Gq): Found in arteries and veins, promotes smooth muscle contraction via IP3/DAG pathway, leading to vasoconstriction.
- β1 (Gs): Primarily in cardiac nodes and ventricles, increases cAMP, leading to increased HR and contractility.
- β2 (Gs): Found in skeletal muscle arteries, increases cAMP, causing smooth muscle relaxation and vasodilation.
- M2 (Gi): Located in cardiac nodes, decreases cAMP, reducing HR.

Endothelial NO Pathway for Vasodilation
Direct muscarinic agonists and sheer stress cause arterial dilation through the endothelial NO pathway. Muscarinic receptors (M3) on endothelial cells are activated by exogenous direct M agonists, leading to NO production, which then diffuses to smooth muscle cells and activates guanylyl cyclase (GC), increasing cGMP and causing vasodilation.

Mechanism of NO-Induced Vasodilation
- Direct Muscarinic Agonist Activation: Activates M3 receptors on endothelial cells.
- Sheer Stress: Increases NO production in endothelial cells.
- NO Production: NO generated in endothelial cells diffuses to smooth muscle cells.
- cGMP Pathway: NO activates GC, increasing cGMP, leading to increased MLCP activity and smooth muscle relaxation (vasodilation).

End Organ Effects of Parasympathetic Activation and Muscarinic Agonists
- Eye: Miosis (pupil constriction) and accommodation for near vision.
- Heart: Decreased HR (M2 receptor activation).
- Blood Vessels: No direct effect from parasympathetic activation but vasodilation through the NO pathway when muscarinic agonists are present.
- Lung: Bronchoconstriction and increased secretion.
- GI/Urinary: Increased motility and voiding.
- Glands: Increased secretion (lacrimation, salivation).

Comparison of Direct and Indirect Cholinomimetics
- Direct Cholinomimetics (e.g., Acetylcholine): Act directly on muscarinic or nicotinic receptors, producing rapid but short-lived effects.
- Indirect Cholinomimetics (e.g., AChE inhibitors): Prolong the action of endogenous acetylcholine by inhibiting its breakdown, leading to sustained activation of cholinergic receptors.
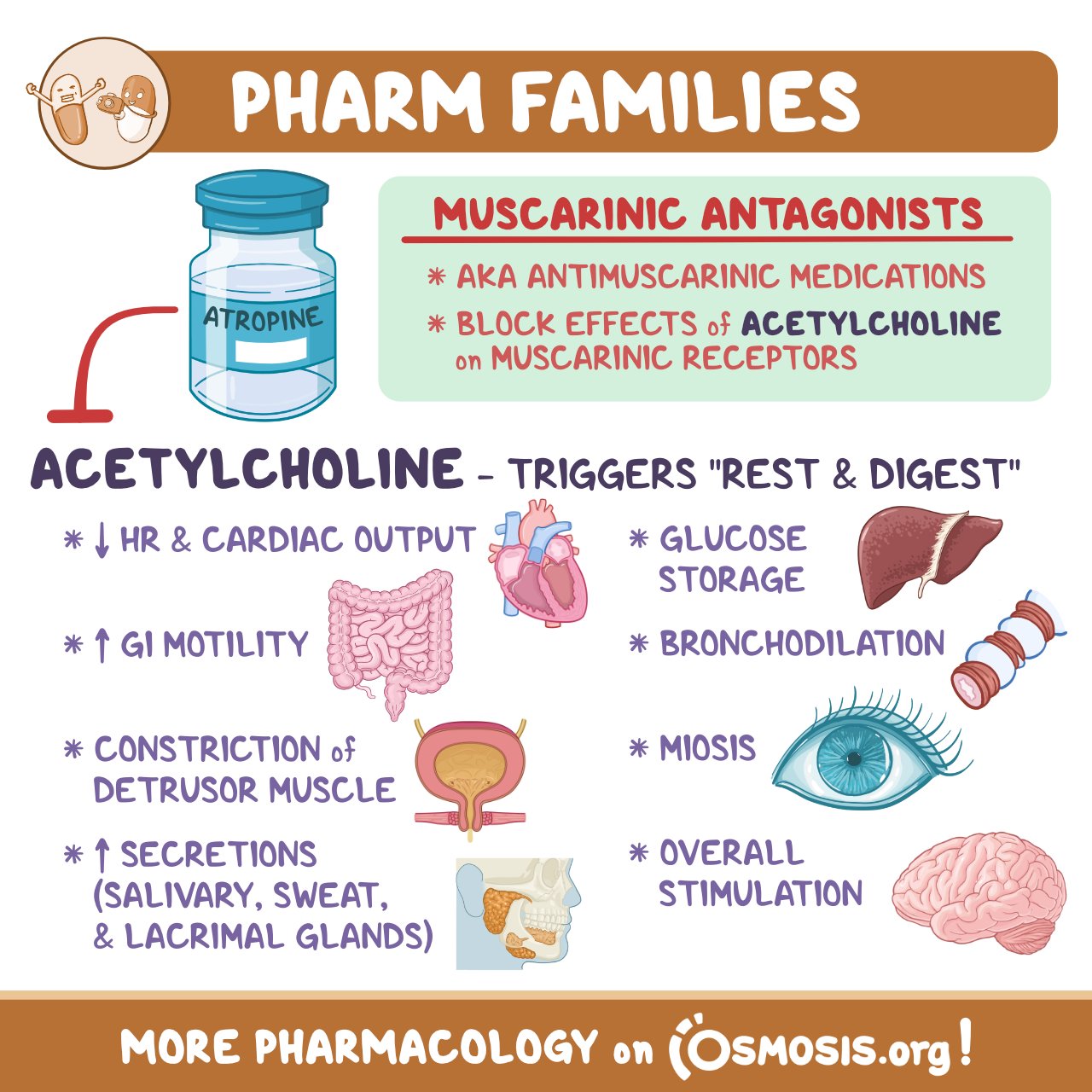
Muscarinic Blockers
- Atropine: Prototypical muscarinic blocker used to increase HR by blocking M2 receptors in the heart. It has no significant effect on blood pressure (BP) since there is no parasympathetic innervation in blood vessels. Atropine also blocks reflex bradycardia induced by increased BP.
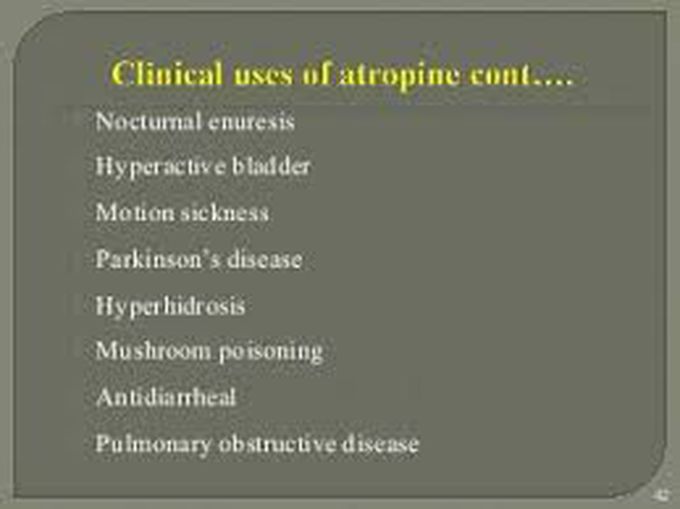
Clinical Uses of Atropine
- Treatment of bradycardia
- Antidote for organophosphate poisoning (AChE inhibitor toxicity)
Predominant Tone and Ganglionic Blockers
- Predominant Tone: Generally, the parasympathetic system dominates most organs except in blood vessels where sympathetic tone prevails.
- Ganglionic Blockers: These drugs (e.g., mecamylamine) block both sympathetic and parasympathetic signaling at the ganglia. The physiological effect depends on the predominant tone of the target tissue. For example, in blood vessels, a ganglionic blocker will cause vasodilation since it blocks the sympathetic tone.