Cardiac Arrhythmias

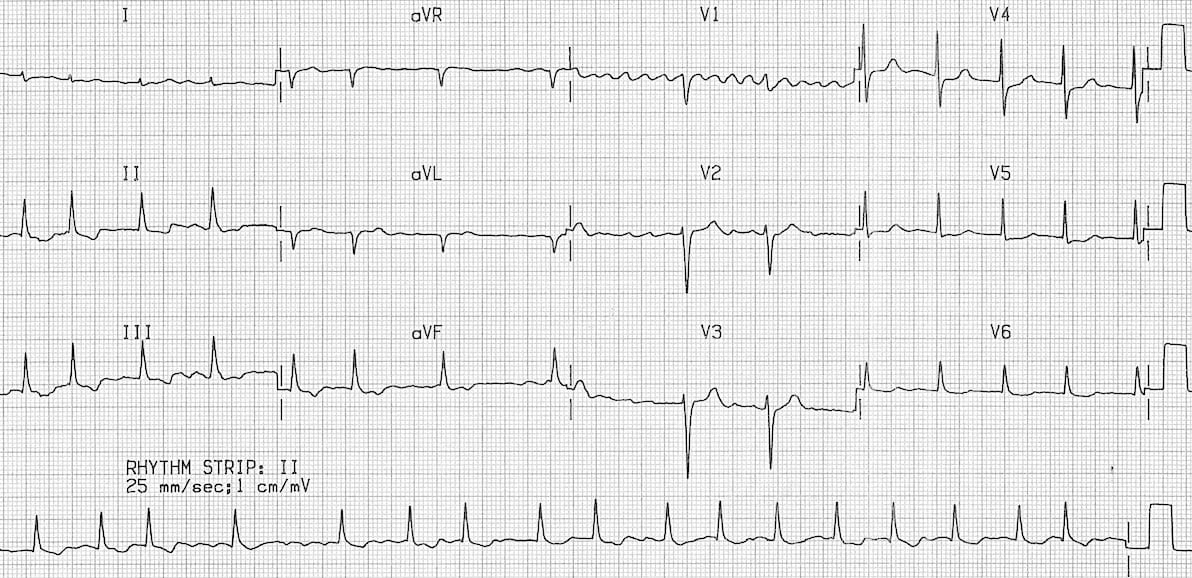
Normal Sinus Rhythm
- P before every QRS & QRS after every P
- P:QRS = 1
- Upright P wave in Leads II, III, AVF (Inferior Leads)
- Equal intervals between identical waves
- P-P interval
- QRS-QRS interval
Sinus Arrhythmia
- Respirophasic variation of sinus rate
- Sinus rate increases during inspiration (withdrawal of parasympathetic tone), decreases with expiration
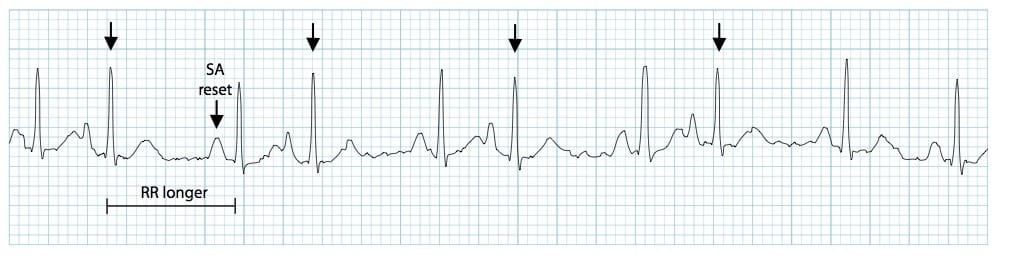
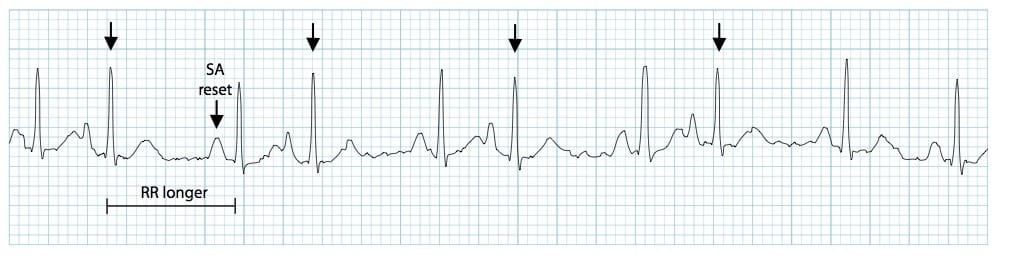
Sinus Pause
- Sinus node dysfunction, often due to age or medications
- No escape rhythm in the pacemaker hierarchy
- May pass out ("syncope")
Atrial Rhythm
- Atrial pacemaker rate is similar to sinus
Junctional Rhythm
- Atrial impulse starts near the AV node and uses the His-Purkinje system
- Based on the location, P waves may be right before, within, or after the QRS
- QRS duration usually normal
- Junctional rhythm 40-60 bpm
- Accelerated junctional rhythm 60-100 bpm
- Junctional tachycardia >100 bpm
- Junctional bradycardia < 40 bpm

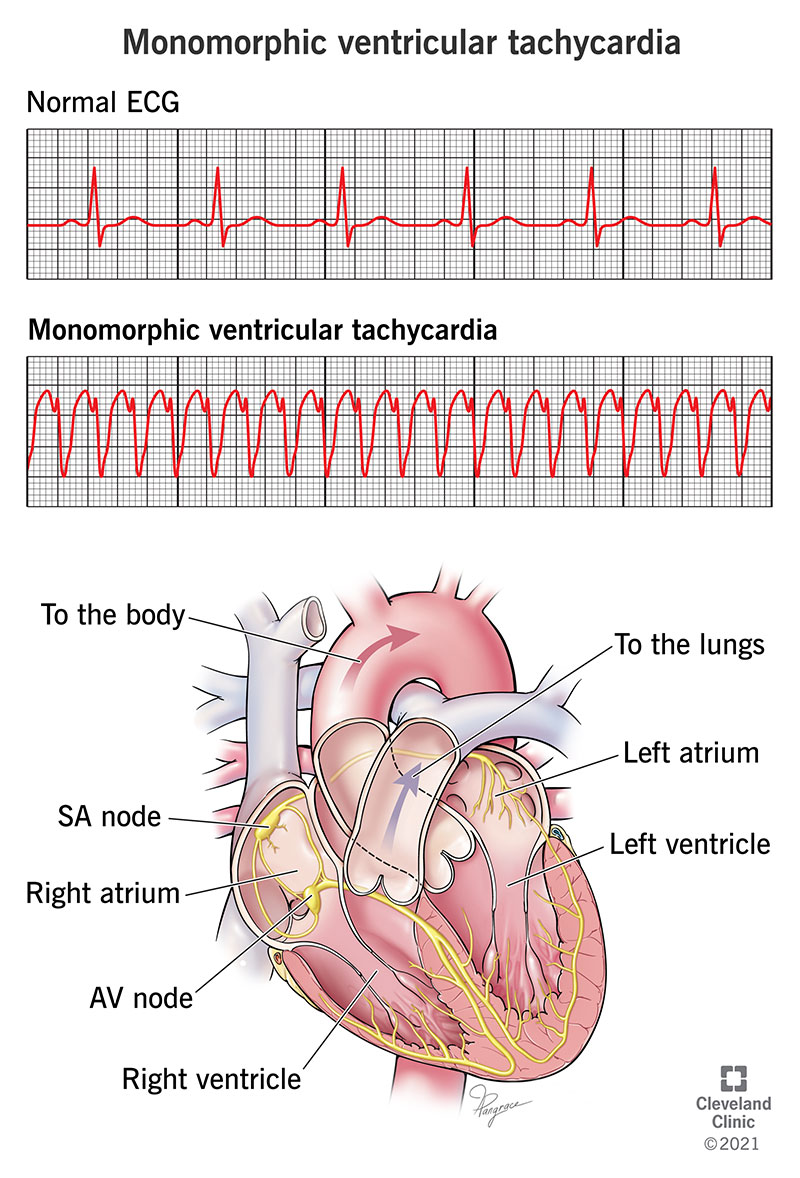
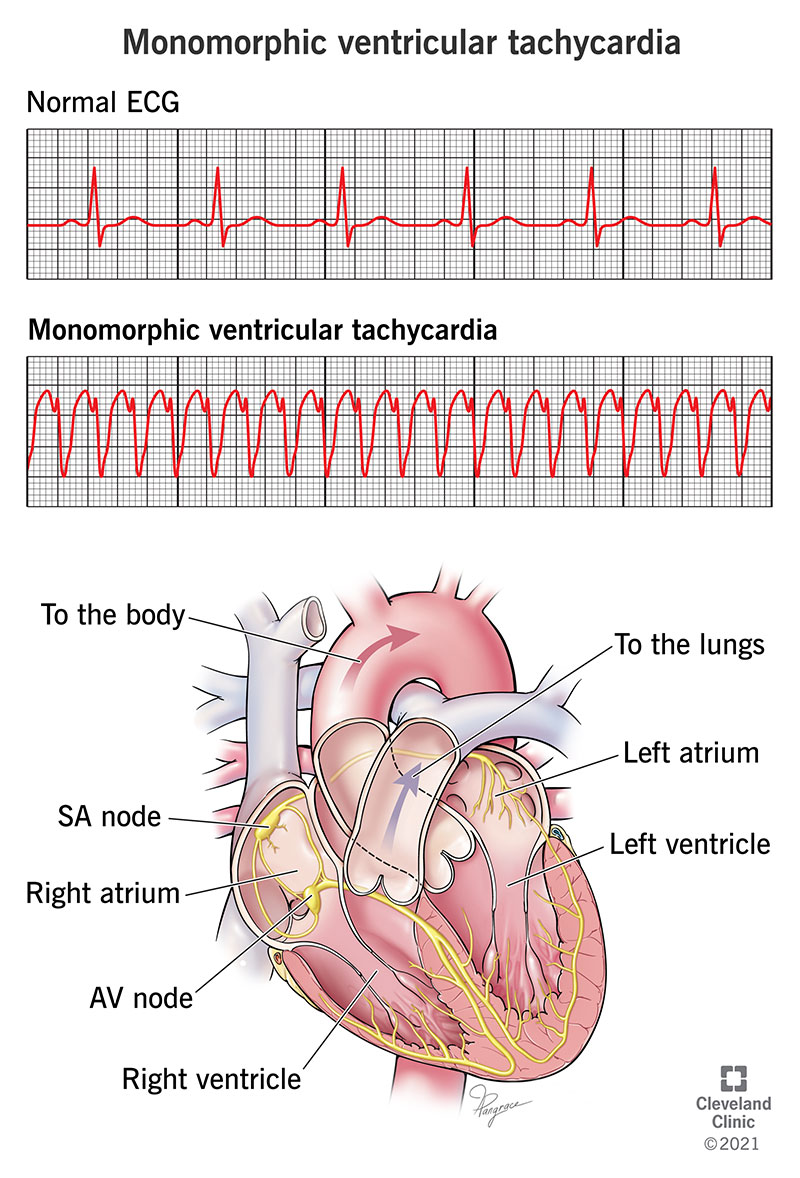
Ventricular Rhythm
- Ventricular escape rhythm 20-40 bpm
- Accelerated idioventricular rhythm 40-100 bpm
- Ventricular tachycardia >100 bpm
Premature Atrial Complex (PAC)
- A complex that occurs before the next expected P wave ("premature") and that originates in the atria (P wave of different morphology than sinus P wave, "atrial complex")
Premature Junctional Complex/Junctional Escape Complex
- Premature Junctional Complex
- Junctional Escape Beat

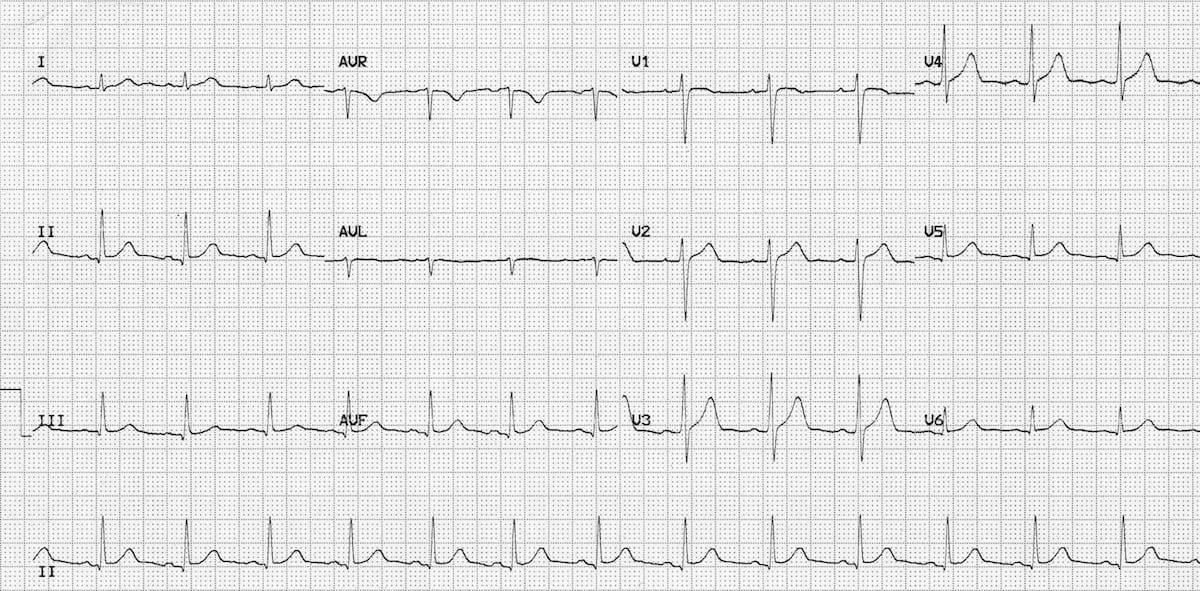
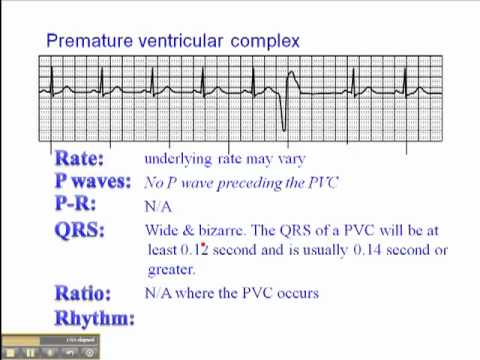
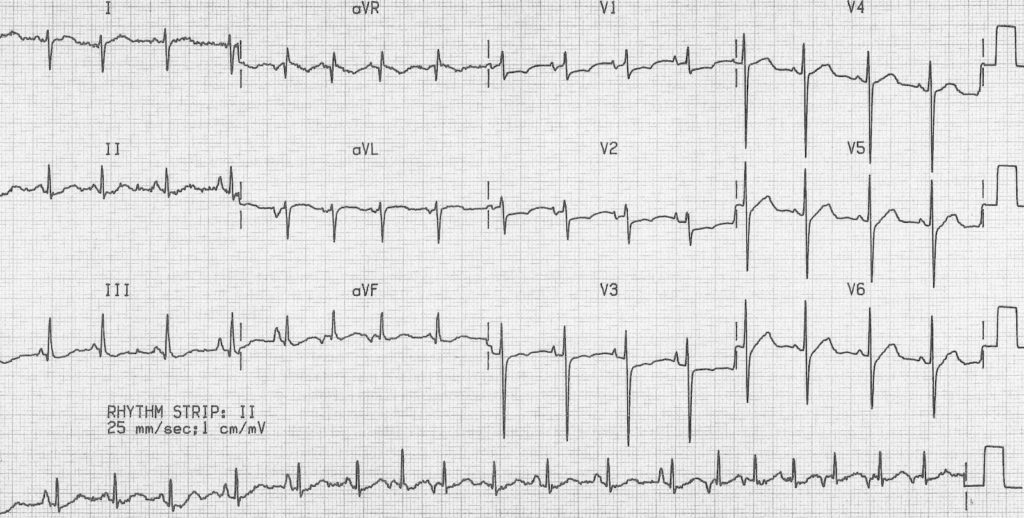
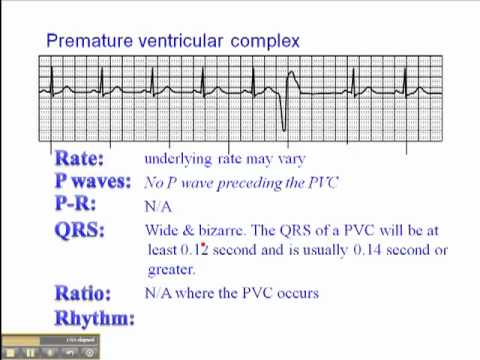
Premature Ventricular Complex (PVC)
- Wide QRS (> 0.120 sec) with abnormal polarity
- No preceding P wave
- Unifocal or Multifocal
Patterns:
- Isolated
- Bigeminy → every second complex is PVC
- Trigeminy → every third complex is PVC
- Quadrigeminy → every fourth complex is PVC
General Approach to Tachyarrhythmias
- Is the QRS complex narrow or wide?
- Is the rhythm regular or irregular?
- Where are the P waves and how do they look?
Narrow-Complex Tachycardia
Regular rhythm
- Morphology same as sinus. Seen in leads II, III, aVF, and V1
- P waves just after the QRS (pseudo R' in lead V1) or no P waves
- Short RP interval
Irregular rhythm
- Flutter waves
- Irregular baseline with no P waves
- At least three different P wave morphologies
[h3]Wide-Complex Tachycardia[/h3]

- Pre-excited tachycardia (antidromic AVRT)
- Supraventricular tachycardia (SVT) with aberrant conduction
- Ventricular tachycardia
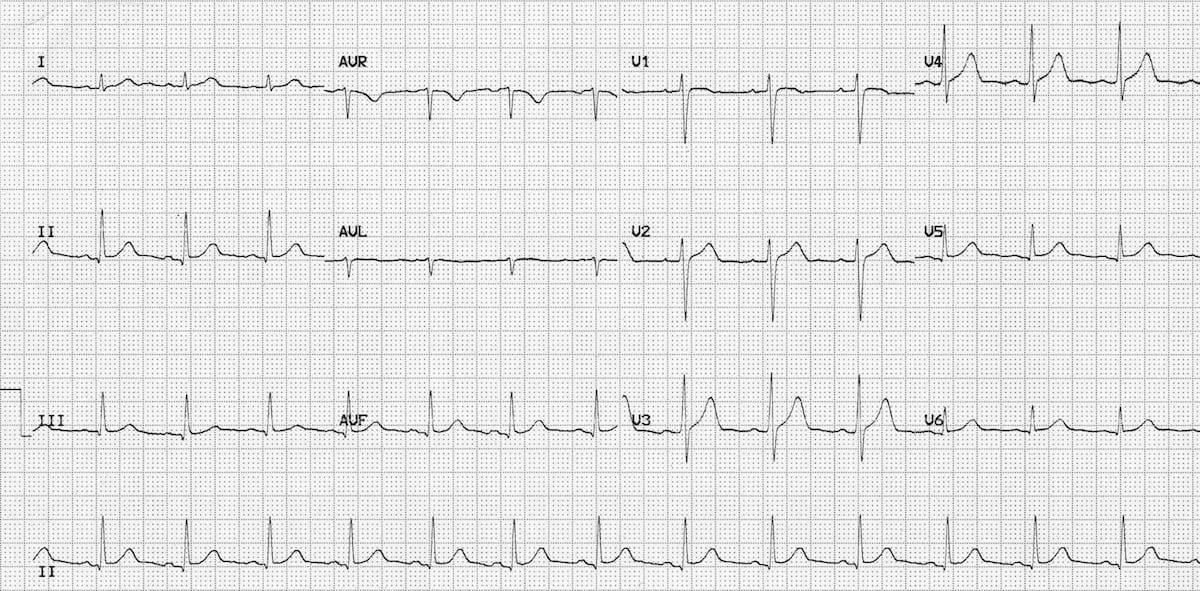
Atrial Fibrillation 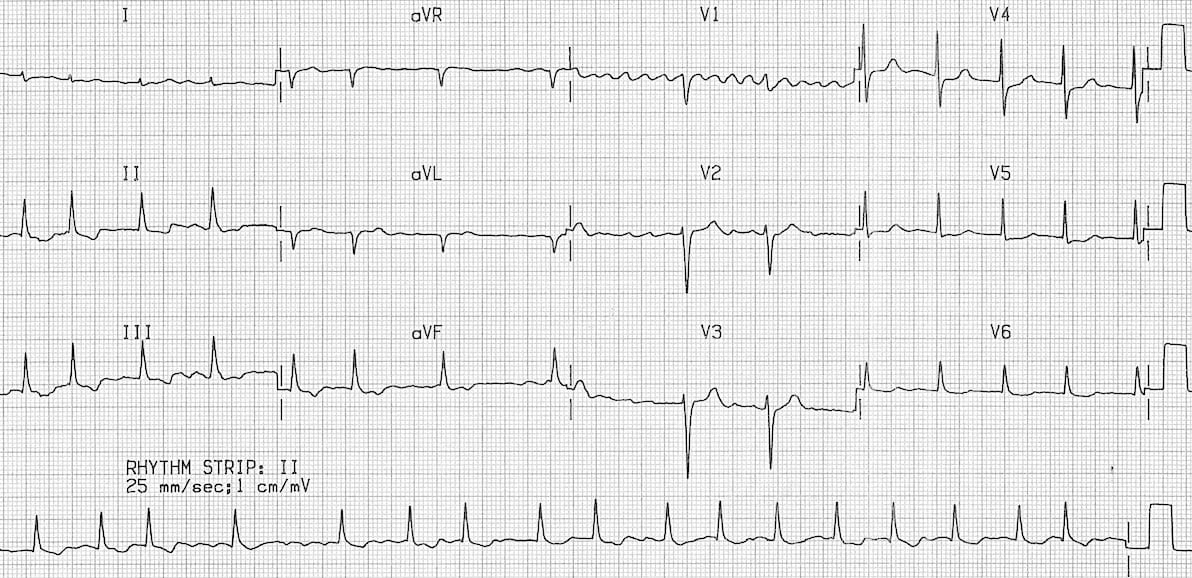
- Irregularly irregular rhythm
- Extremely fast atrial rate with sporadic conduction through AV node
- No obvious P waves; irregular baseline
- A. Fib with rapid ventricular response (RVR): Rate > 100
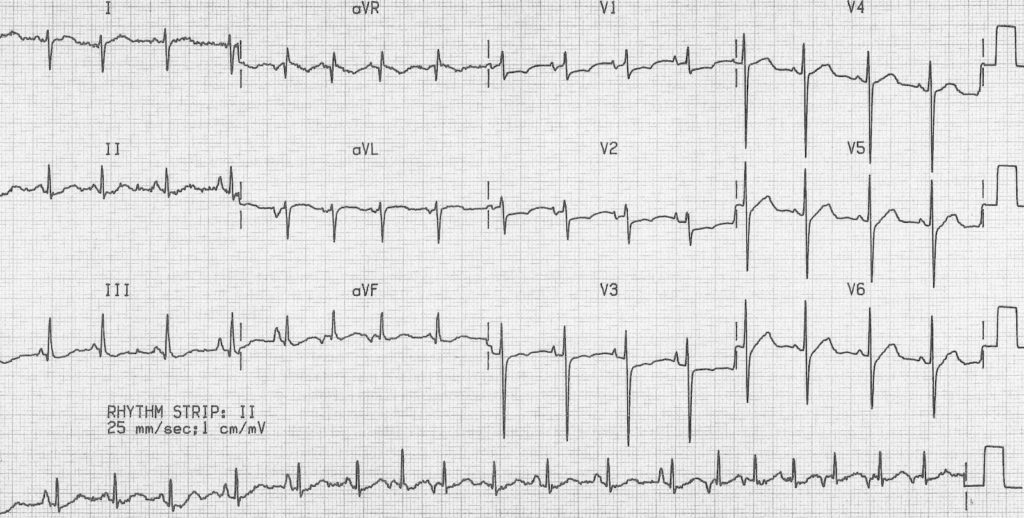
Abnormal P Waves: Atrial Flutter

- Atria depolarizing at ~300 bpm
- Saw-tooth appearance
- AV node controls ventricular conduction, often 2:1, 3:1, 4:1 or variable conduction
- Usually regular, irregular if variable conduction
Multifocal Atrial Tachycardia
- Three or more P wave morphologies
- Common in patients with lung disease
[h2]Supraventricular Tachycardias (SVT)[/h2]

- Generally a narrow complex tachyarrhythmia that is not sinus tachycardia/atrial fibrillation/atrial flutter
- Re-entry is the mechanism of most SVT