Acute Coronary Syndrome
Acute Coronary Syndrome

Intima
- Media
- Smooth muscle cells
- Endothelium
- Adventitia
Normal Artery
Early Atheroma
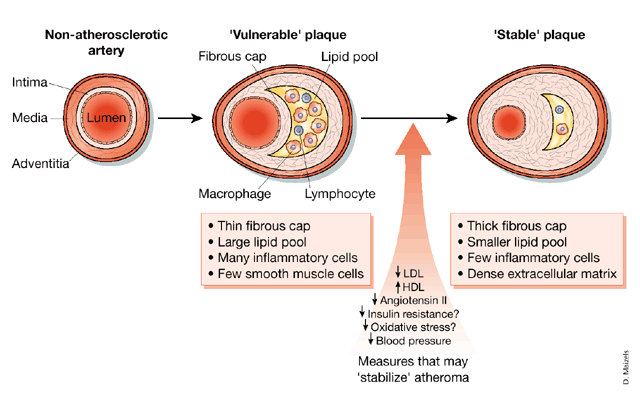
'Stabilized' Plaque
- Small lipid pool
- Healed ruptured plaque
- Thick fibrous cap
- Narrow lumen
Vulnerable Plaque
- Thin fibrous cap
- Large lipid pool
- Many inflammatory cells

Ischemic Heart Disease: It’s a Spectrum!
Unstable Angina
Shares common underlying pathophysiology with non-STEMI (NSTEMI) and STEMI. Clinically presents as new onset chest pain, rest pain or an increase in frequency/duration of previously occurring anginal episodes. Ischemic events are not associated with irreversible myocardial tissue damage. Associated with partial thrombus occlusion.

Non-ST Elevation MI (NSTEMI)
Associated with chest discomfort at rest that typically lasts more than 20 minutes. Partial/complete occlusion of the lumen by thrombus causes tissue damage and necrosis (infarction). Often associated with ST depression on ECG. Typically, worse prognosis than unstable angina.
ST Elevation MI (STEMI)Characterized by complete occlusion of an epicardial coronary artery. Damage to the myocardium is dependent upon the duration of the occlusion. Associated with ST elevation and high troponin levels. Severe symptoms and life-threatening complications may occur.
Extent of Necrosis
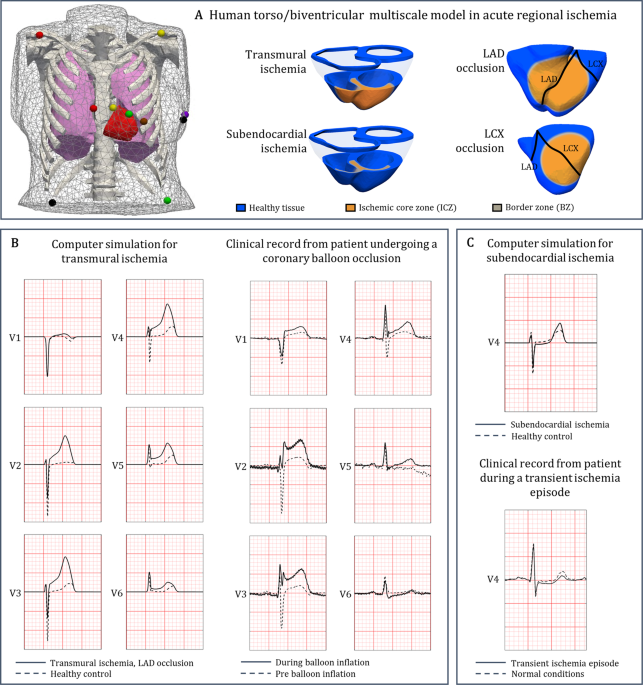
Subendocardial Ischemia
Subendocardial tissue is thought to be vulnerable to ischemia/infarct secondary to high contractile pressures, fewer collaterals, etc.
Transmural IschemiaThe extent of necrosis is typically related to the amount of muscle supplied by the occluded vessel, how long the flow is impaired in the vessel, oxygen demand, and the presence of collaterals.

Pathologic Time Line in Transmural Infarction
Early Changes
- 1-2 min: ATP levels fall; cessation of contractility.
- 10 min: 50% depletion of ATP; cellular edema, decreased membrane potential, and susceptibility to arrhythmias.
- 20-24 min: Irreversible cell injury.
- 1-3 h: Wavy myofibers.
- 4-12 h: Hemorrhage, edema, PMN infiltration begins.
- 18-24 h: Coagulation necrosis (pyknotic nuclei with eosinophilic cytoplasm), edema.
- 2-4 d: Total coagulation necrosis (no nuclei or striations, rimmed by hyperemic tissue); monocytes appear; PMN infiltration peaks.
Late Changes
- 5-7 d: Yellow softening from the resorption of dead tissue by macrophages.
- 7+ d: Granulation tissue forms, ventricular remodeling.
- 7 wk: Fibrosis and scarring complete.
Consequences of Coronary Thrombosis
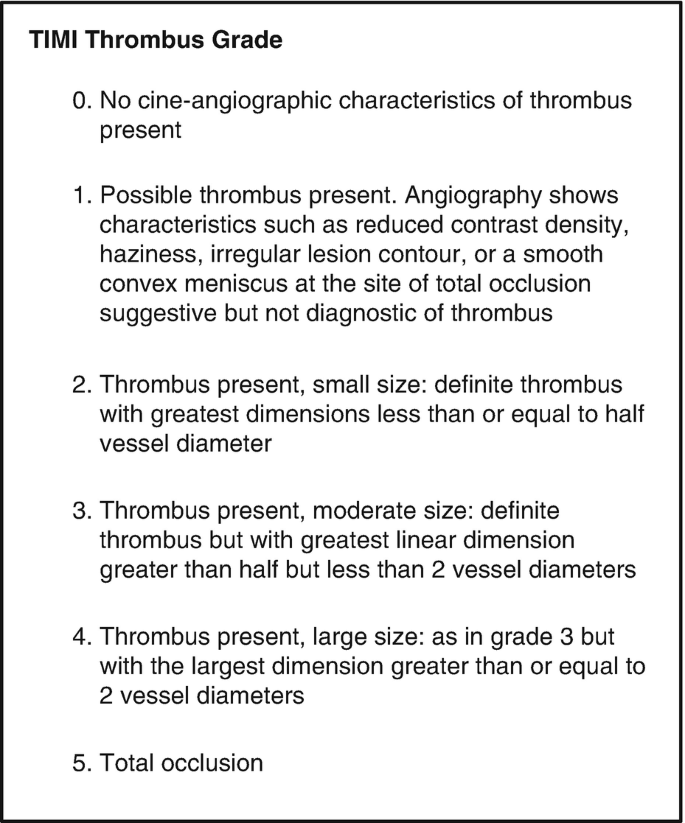
Coronary Thrombus
- Small thrombus (non-flow-limiting)
- ST segment depression and/or T wave inversion.
- Serum biomarkers.
- Unstable angina.
- Non-ST-segment elevation MI.