Dyslipidemia and Lipoprotein Metabolism
Dyslipidemia and Lipoprotein Metabolism
Learning Objectives:
- Describe the basics of lipoprotein and cholesterol metabolism, manifestations of abnormal metabolism, and their relationship to cardiovascular disease.
- Know the prototype drugs used to treat hyperlipoproteinemias, including their mechanisms of action, clinical uses, contraindications, and major adverse effects.
Lipoprotein Metabolism
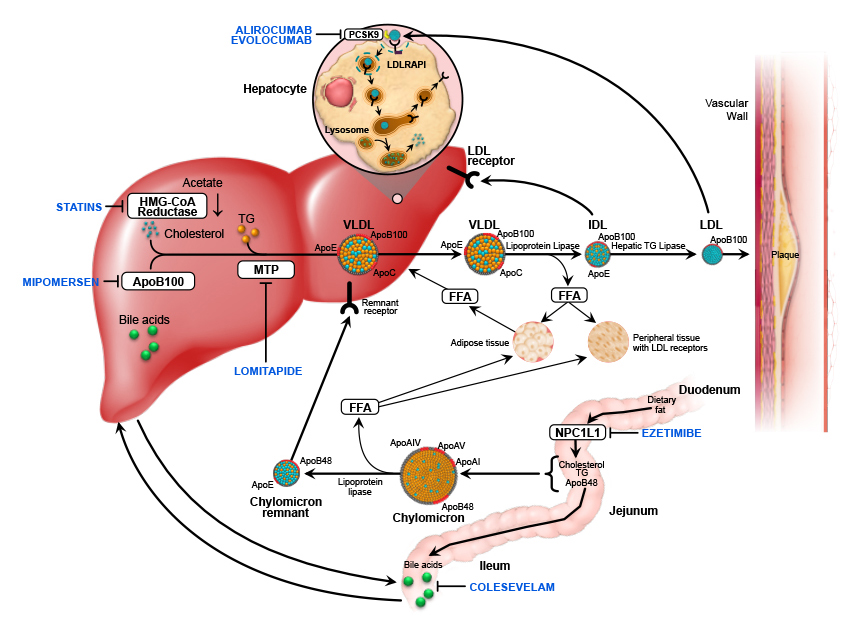
Lipoproteins are complex particles composed of multiple proteins, commonly found in the bloodstream, tasked with transporting lipids (fats), such as triglycerides and cholesterol. Here are the essential aspects of lipoprotein metabolism:
- Dietary fats are absorbed through the intestines and packaged into chylomicrons.
- Chylomicrons deliver triglycerides to tissues like adipose (fat) tissue and muscle. The remnants are then taken up by the liver.
- The liver synthesizes Very Low-Density Lipoproteins (VLDL), which after the loss of triglycerides, become Intermediate-Density Lipoproteins (IDL) and eventually Low-Density Lipoproteins (LDL).
- LDL is often referred to as "bad cholesterol" because elevated levels contribute to plaque formation that narrows and hardens the arteries.
- High-Density Lipoproteins (HDL) is known as "good cholesterol" as it assists in removing cholesterol from the arteries and transporting it back to the liver for excretion or re-utilization.

Definitions of Dyslipidemia
- Hyperlipoproteinemia / Hyperlipidemia: Elevated serum cholesterol- or triglyceride-carrying lipoproteins.
- Hypercholesterolemia: Elevated levels of total serum cholesterol.
- Hypertriglyceridemia: Elevated levels of total serum triglycerides.
- Combined/mixed hyperlipidemia: Elevated serum cholesterol and triglycerides.
Causes of Hyperlipidemia
Primary Causes
Primary hyperlipidemia is typically genetic in origin and can include:
- Familial Hypercholesterolemia: Mutations in genes like LDL receptor, ApoB, PCSK9, leading to decreased ability to metabolize LDL. Can be homozygous (LDL > 465 mg/dL) or heterozygous (LDL > 250 mg/dL).
- Manifestations include:
- Xanthomas: Plaques or nodules composed of lipid-laden histiocytes in skin, especially around the eyelids (xanthelasma).
- Tendinous xanthoma: Lipid deposits in tendons, especially the Achilles tendon.
- Corneal arcus: Lipid deposits in the cornea.
- Hypertriglyceridemia: Frequently caused by apolipoprotein C-II or lipoprotein lipase deficiencies, impeding lipoprotein catabolism.
Secondary Causes
Secondary factors contributing to dyslipidemia include:
- Hypertriglyceridemia: Conditions such as diabetes mellitus, hypothyroidism, alcohol ingestion, and corticosteroid excess.
- Hypercholesterolemia: Conditions like severe nephrosis, cholestasis, hypothyroidism, glycogen storage disease, and anorexia nervosa.
Complications of Hyperlipidemia
- Atherosclerotic Vascular Disease (ASVD): Systemic disease characterized by plaque formation in the vasculature resulting in conditions like coronary artery disease (CAD), cerebral vascular disease (CVD), renovascular disease (RVD), and peripheral artery disease (PAD). It is strongly associated with hypercholesterolemia.
- Pancreatitis: Severe elevations in triglycerides (>500 mg/dL) are associated with pancreatitis, necessitating treatment.
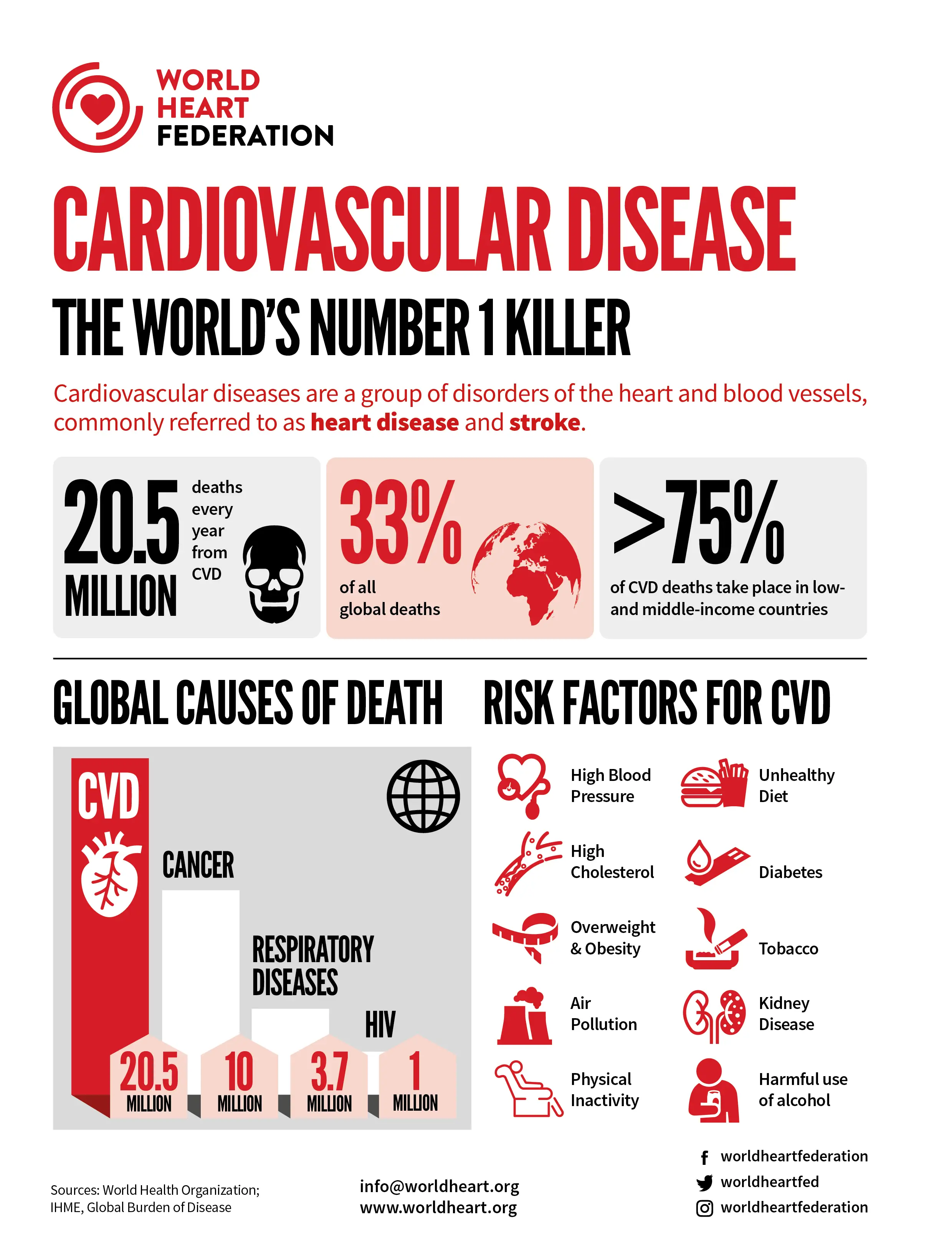
Association Between Lipoproteins and Coronary Artery Disease (CAD)
- HDL: Considered protective (the higher, the better). Elevated HDL levels reduce the risk of CAD.
- LDL: Known as bad cholesterol (the higher, the worse). Elevated LDL levels increase the risk of CAD.
Antihyperlipidemic Therapy
Principles
- Dietary and behavioral modifications: Therapeutic lifestyle changes should be attempted first. This includes reducing secondary causes and incorporating fish oil to reduce triglycerides by 25-30%.
- Pharmacological intervention: Based on risk assessment using tools like ASCVD-Risk-Estimator-Plus. Define the risk, goal, and therapy accordingly.
- Primary goal: Prevent atherosclerosis by reducing plaque formation, stabilizing existing plaques, and potentially reversing plaque formation.
HMG-CoA Reductase Inhibitors (Statins)
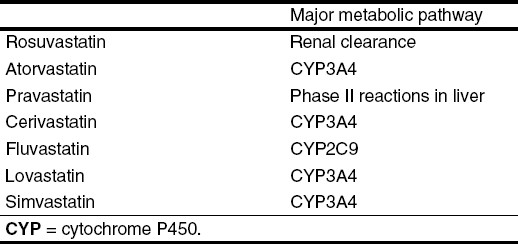
- Mechanism: Competitive inhibitors of HMG-CoA reductase that reduce hepatic cholesterol synthesis, thereby increasing LDL receptor expression and decreasing circulating LDL.
- Effects: Decrease LDL by up to 55%, increase HDL by 15%, and modestly decrease triglycerides.
- Clinical Applications: Used in both primary and secondary prevention of atherosclerotic vascular disease and in treating hypercholesterolemia.
- Adverse Effects: Common effects include myalgia and gastrointestinal issues. Rare but serious effects include rhabdomyolysis and liver toxicity.

PCSK9 Inhibitors
- Drugs: Alirocumab, Evolocumab
- Mechanism of Action: These are monoclonal antibodies that inhibit PCSK9, thereby increasing the number of LDL receptors and reducing LDL levels.
- Effects: Decrease LDL up to 75% when used with statins.
- Clinical Use: Adjuvant to diet and statin therapy for familial hypercholesterolemia or established atherosclerotic CVD.
- Adverse Effects: Generally well-tolerated with minor effects such as injection site reactions.
Selective Cholesterol Absorption Inhibitors
- Drug: Ezetimibe
- Mechanism of Action: Inhibits NPC1L1-mediated absorption of cholesterol in the small intestine.
- Effects: Decreases LDL up to 20%, minimal effect on HDL and triglycerides.
- Clinical Use: Primary hypercholesterolemia especially where statins are not sufficient or contraindicated.
- Adverse Effects: Diarrhea, elevated liver enzymes when co-administered with statins.

Bile Acid Sequestrants
- Drugs: Cholestyramine, Colesevelam, Colestipol
- Mechanism of Action: Bind bile acids in the intestine, promoting conversion of cholesterol to bile acids in the liver.
- Effects: Decrease LDL up to 25%, small HDL increase, and increases TG levels.
- Clinical Use: When statins are not sufficient or contraindicated. Colesevelam is also used to reduce HbA1C in Type 2 diabetes.
- Adverse Effects: Gastrointestinal issues, increase in triglycerides, and decreased absorption of other drugs and vitamins.
Fibrates
- Drugs: Fenofibrate, Gemfibrozil
- Mechanism of Action: Ligands for PPARα that regulate fatty acid metabolism genes.
- Effects: Decrease triglycerides up to 70%, with modest HDL increase and LDL decrease.
- Clinical Use: Primarily for hypertriglyceridemia and metabolic syndrome.
- Adverse Effects: Gallstones, myopathy, and elevated liver enzymes.

Niacin (Nicotinic Acid)
- Mechanism of Action: Decreases fatty acid release from adipose tissue, inhibits triglyceride synthesis in the liver, and increases HDL.
- Effects: Decreases triglycerides up to 45%, modest LDL decrease, and HDL increase up to 35%.
- Clinical Use: Isolated low HDL or in familial combined hyperlipidemia.
- Adverse Effects: Flushing, pruritus, hyperuricemia, impaired insulin sensitivity, and hepatotoxicity.
Combination Therapy
Combining drugs with different mechanisms can produce additive effects but must consider the benefits versus risk. Common combinations include:
- Statin + Ezetimibe
- Statin + PCSK9 inhibitor
- Statin + Bile Acid Sequestrant
Conclusion: Effective management of hyperlipidemia involves an understanding of the underlying causes and appropriate use of different classes of lipid-lowering agents to mitigate the risk of cardiovascular disease.