Congenital and Atherosclerotic Vascular Disease
Congenital and Atherosclerotic Vascular Disease
Lesson Objectives
1. Describe the common congenital vascular abnormalities and their potential effects on patient health
Congenital vascular abnormalities are defects in blood vessels that arise during fetal development. Common types include:
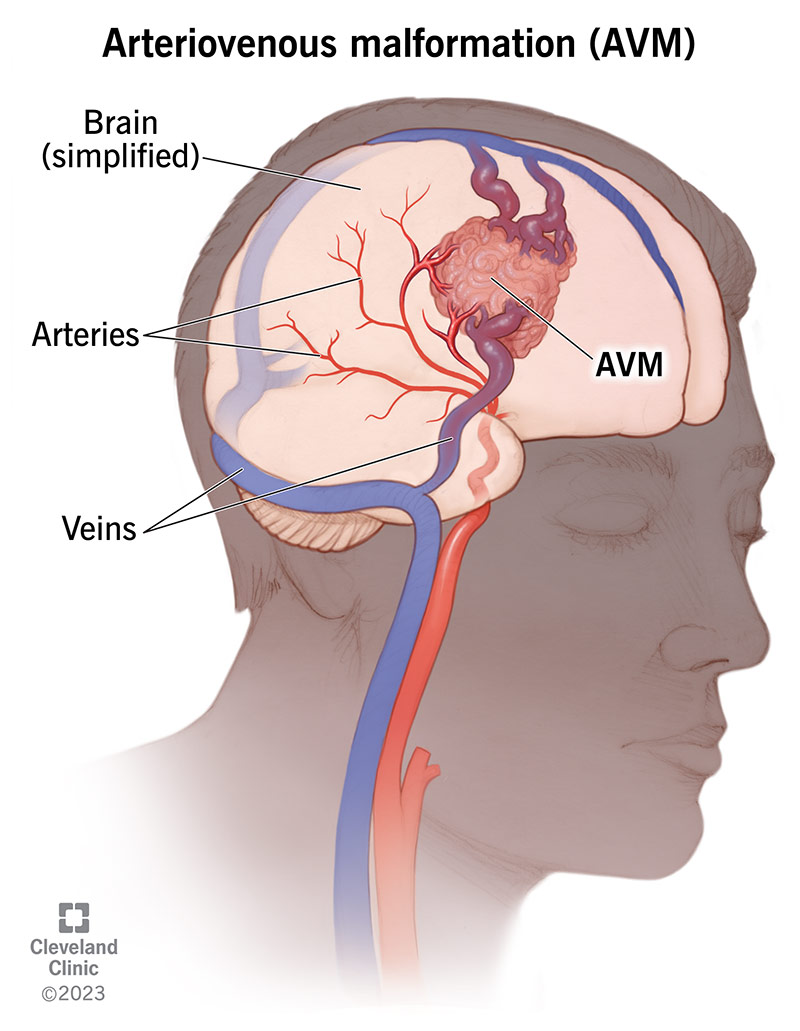
Arteriovenous malformations (AVMs): These are abnormal connections between arteries and veins, bypassing the capillary system. AVMs can lead to hemorrhage, seizures, or other neurological symptoms depending on their location.
Coarctation of the aorta: This is a narrowing of the aorta, which can increase the workload on the heart, leading to hypertension or heart failure if left untreated.
Berry aneurysms: Small saccular aneurysms, often found in the brain's circle of Willis, can rupture and cause subarachnoid hemorrhage, which is a life-threatening condition.
These abnormalities can have varying effects on patient health, from asymptomatic to life-threatening, depending on the size, location, and nature of the abnormality.
2. Describe how vessel wall cells respond to injury
When a blood vessel is injured, a complex cascade of events occurs involving endothelial cells, smooth muscle cells, and the extracellular matrix. Key responses include:
Endothelial injury: When endothelial cells are damaged (e.g., due to hypertension, smoking, or high cholesterol), they lose their normal protective functions. This can lead to increased permeability, inflammation, and the attraction of circulating inflammatory cells.
Smooth muscle cell migration: In response to injury, smooth muscle cells from the media layer migrate to the intima (the innermost layer) and begin proliferating. This results in thickening of the vessel wall, which can contribute to atherosclerosis.
Inflammation: Inflammatory cells like monocytes and lymphocytes are recruited to the site of injury, where they release cytokines and growth factors, further promoting smooth muscle cell proliferation and matrix production.
Extracellular matrix deposition: Fibrous tissue and extracellular matrix components are laid down as part of the healing process, leading to potential thickening and loss of elasticity in the vessel wall, which can contribute to vascular disease.
3. List the risk factors in atherosclerosis and describe how they may contribute to atheroma formation
Risk factors for atherosclerosis include:
- Hyperlipidemia: High levels of low-density lipoprotein (LDL) cholesterol promote the accumulation of lipid in the arterial wall, forming the fatty streaks that precede atheroma.
- Hypertension: High blood pressure can cause endothelial injury, which makes the vessels more susceptible to lipid deposition and inflammatory processes.
- Smoking: Cigarette smoke damages the endothelium and increases oxidative stress, both of which contribute to the initiation and progression of atherosclerosis.
- Diabetes: High blood sugar levels increase oxidative stress and inflammation, further damaging the vessel walls and accelerating atherosclerosis.
- Age and gender: The risk of atherosclerosis increases with age, and men are at higher risk than pre-menopausal women due to protective effects of estrogen.
- Family history: Genetic predispositions to hypercholesterolemia or hypertension can increase the risk of developing atherosclerosis.
Each of these risk factors either causes endothelial injury or promotes lipid accumulation, inflammation, and smooth muscle cell proliferation, contributing to the formation of atheromas.
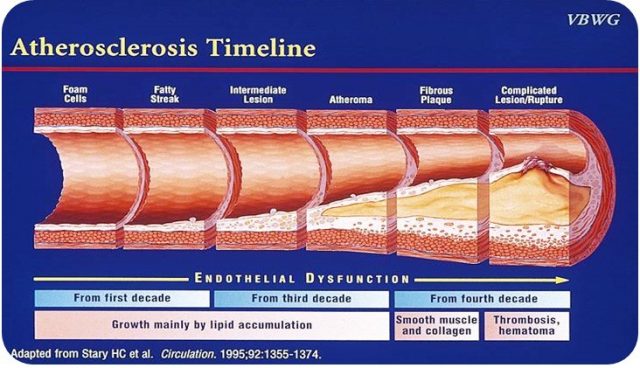
4. Outline the sequence of events in atheroma formation
Atheroma formation involves the following stages:
- Endothelial injury: Damage to the endothelial lining of blood vessels initiates the process.
- Lipid accumulation: LDL cholesterol enters the vessel wall and undergoes oxidation, which promotes further endothelial damage.
- Inflammatory cell recruitment: Monocytes and other immune cells are recruited to the site of injury and differentiate into macrophages, which engulf oxidized LDL and become foam cells.
- Fatty streak formation: Foam cells accumulate in the intima, forming a visible fatty streak in the vessel wall.
- Smooth muscle proliferation: Smooth muscle cells from the media migrate to the intima and proliferate, producing extracellular matrix and forming a fibrous cap over the growing atheroma.
- Plaque formation: As the plaque enlarges, it can encroach on the vessel lumen, restricting blood flow. It also becomes prone to rupture, which can lead to thrombosis and vascular occlusion.

5. Describe causes, types, pathogenesis, and clinical course of aortic aneurysms
Causes: The most common causes of aortic aneurysms include atherosclerosis, genetic connective tissue disorders (e.g., Marfan syndrome, Ehlers-Danlos syndrome), and infections (e.g., syphilitic aortitis).
Types:
- Abdominal aortic aneurysm (AAA): Occurs below the renal arteries and is usually associated with atherosclerosis. It predominantly affects elderly men and can be asymptomatic until rupture.
- Thoracic aortic aneurysm (TAA): Affects the aorta in the chest, often associated with genetic conditions (e.g., Marfan syndrome) or long-standing hypertension.
Pathogenesis: Aortic aneurysms develop due to weakening of the vessel wall, often as a result of chronic inflammation, degradation of the extracellular matrix, or genetic defects affecting the structural integrity of the wall. As the wall weakens, the aorta dilates, leading to the risk of rupture.
Clinical course: Aortic aneurysms are often asymptomatic until they become large enough to cause pain, a pulsatile mass, or symptoms due to compression of adjacent structures. The most serious complication is rupture, which can lead to life-threatening hemorrhage. Rupture risk increases with aneurysm size.
Congenital Anomalies
Blood Vessels Aberrant (Anomalous) Anatomy
Berry Aneurysms (Cerebral)
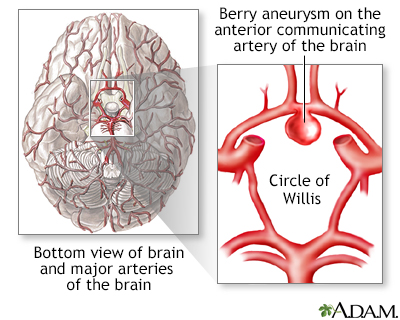
Berry aneurysms are aneurysmal dilatations of the cerebral arteries. A key characteristic is the presence of the entire vessel wall forming the aneurysm (true aneurysm) with a general lack of degenerative changes and atherosclerosis usually seen in acquired aneurysms.
Clinical Correlation: A 45-year-old male is admitted to the emergency department with the worst headache of his life, quickly loses consciousness, codes, and dies due to the rupture of a saccular aneurysm.
Arteriovenous (AV) Malformations

Arteriovenous malformations lack a capillary bed and may occur congenitally or result from the rupture of an arterial aneurysm into an adjacent vein, penetrating injuries, inflammatory necrosis of vessel walls, or iatrogenic situations (e.g., hemodialysis). Clinically significant due to the potential for high-output cardiac failure and risks of rupture and hemorrhage, especially in the brain.
Fibromuscular Dysplasia

Fibromuscular dysplasia is characterized by focal irregular thickening of medium to large vessels like renal and carotid arteries. It consists of irregular medial and intimal hyperplasia and is considered developmental or congenital. It is an important cause of renovascular hypertension in young individuals, resulting in decreased blood flow, renin release, and hypertension.
Vessel Wall Cells Response to Injury
Vessel Development, Growth, and Remodeling
Vessel growth is a complex interaction between endothelial and smooth muscle cells, creating new vessels via angiogenesis, essential for tissue perfusion in ischemic conditions and contributing to pathogenesis in tumor growth, arthritis, and diabetic retinopathy.
Endothelial Cells
- Maintenance of permeability barrier
- Elaboration of anticoagulant, antithrombotic, fibrinolytic regulators
- Elaboration of prothrombotic molecules
- Extracellular matrix production
- Modulation of blood flow and vascular reactivity
- Regulation of inflammation and immunity
- Regulation of cell growth
Endothelial Cell Activation

Activators: Cytokines, bacterial products, hemodynamic forces, lipid products, viruses, hypoxia. Induced Genes: Adhesion molecules, cytokines/chemokines, growth factors, vasoactive mediators, coagulation proteins, etc.
Vascular Smooth Muscle Cells
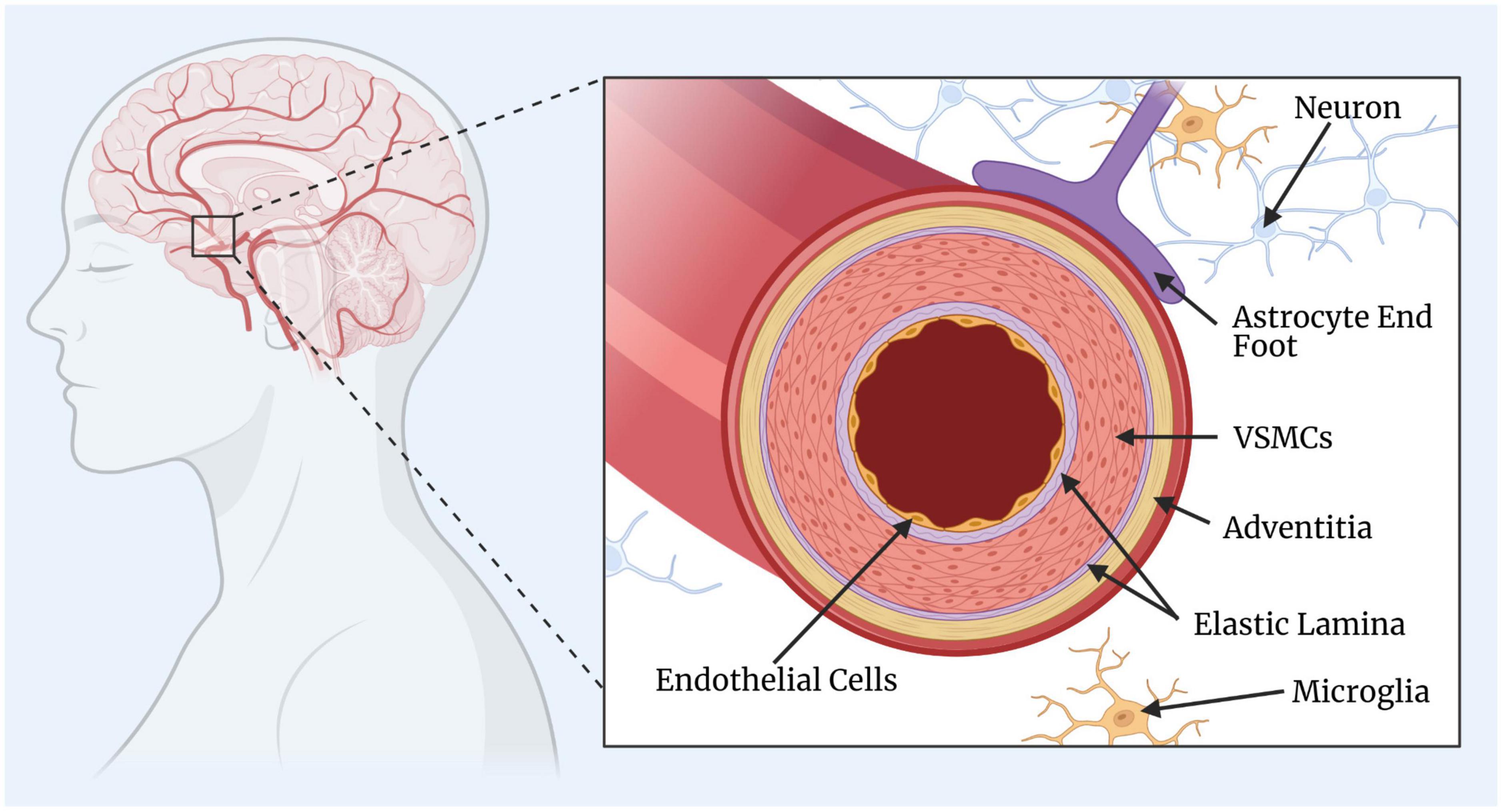
- Constriction and relaxation (vasoconstriction and vasodilation)
- Synthesis of collagen, elastin, proteoglycans, growth factors, cytokines
- Migration to intima and proliferation in response to injury (regulated by growth promoters and inhibitors)
- Formation of neointima after injury response
Atherosclerosis

Pathogenesis
- Begins with endothelial cell injury at areas of disturbed or turbulent flow (e.g., vessel branching points).
- Inflammation initiated by expression of VCAM-1, adhesion, and migration of monocytes, production of ROS, and LDL oxidation.
- Lipids, particularly LDL, oxidized LDL, and Lp(a), play a significant role.
- Smooth muscle cell activation leads to intimal thickening and plaque formation.
Manifestations and Complications
- Ischemic heart disease (angina, myocardial infarction)
- Cerebrovascular disease (stroke)
- Peripheral artery disease (claudication, limb ischemia)
- Renal artery disease (hypertension, renal failure)
- Aneurysms (aortic aneurysm)
Intimal Thickening

- Process begins with vascular injury leading to smooth muscle cell migration to the intima, proliferation, and extracellular matrix synthesis.
- Exaggerated response leads to intimal thickening and potential vessel stenosis or occlusion.
Prevention and Treatment

- Prevention: Stopping smoking, controlling hypertension, exercising, decreasing total & LDL cholesterol, increasing HDL cholesterol.
- Treatment: Lipid-altering therapies (statins, niacin, fibric acid derivatives, cholesterol absorption inhibitors, bile acid-binding agents).