Anti-Arrhythmic Drugs
Anti-Arrhythmic Drugs
Learning Objectives
- Describe the basic strategies in treating different arrhythmias based on their origin.
- Explain how channel blockers work.
- Compare and contrast the four major antiarrhythmic drug classes in their mechanisms of action and indications:
- List prototype drugs, clinical uses, side effects, and toxicities in the four major AA classes.
- List other AA drugs and describe mechanisms of action, clinical uses, side effects, and toxicities.

Cardiac Action Potential
Nodes: SA & AV Nodes
The cardiac action potential in the SA and AV nodes involves several phases:
- Phase 4: Slow depolarization due to If (funny) channels.
- Phase 0: Rapid depolarization due to Ca++ influx.
- Phase 3: Repolarization due to K+ efflux.

Myocytes: Atrial and Ventricular Myocytes
The cardiac action potential in myocytes includes these phases:
- Phase 0: Rapid depolarization due to Na+ influx.
- Phase 1: Initial repolarization due to transient outward K+ current.
- Phase 2: Plateau phase due to balance between Ca++ influx and K+ efflux.
- Phase 3: Repolarization due to K+ efflux.
- Phase 4: Resting membrane potential.
Basic Antiarrhythmic Drug Action
Different antiarrhythmic drugs target different phases of the cardiac action potential:
- Class I (NCB - Na+ Channel Blockers): Target Phase 0 in myocytes.
- Class II (BB - Beta Blockers): Target Phase 4 in nodes.
- Class III (KCB - K+ Channel Blockers): Target Phase 3 in myocytes.
- Class IV (CCB - Ca++ Channel Blockers): Target Phase 0 in nodes.
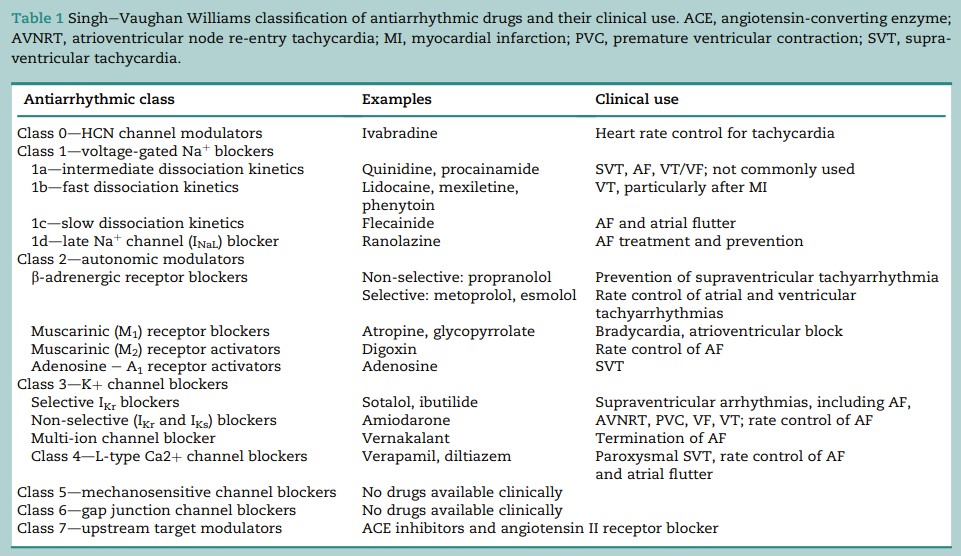
Antiarrhythmic Classes and their Actions
Class I (Na+ Channel Blockers)
- IA (e.g., Quinidine, Procainamide, Disopyramide): Moderate Na+ channel blockade, lengthen AP duration, and increase ERP. Used for atrial and ventricular arrhythmias and WPW syndrome.
- IB (e.g., Lidocaine, Mexiletine): Weak Na+ channel blockade, shorten AP duration, and decrease ERP. Used for acute ventricular arrhythmias, particularly post-MI or digitalis-induced.
- IC (e.g., Flecainide, Propafenone): Strong Na+ channel blockade, no effect on AP duration, and may be proarrhythmic. Used as a last resort for refractory VT.
Adverse Effects of Class I Drugs
- IA: Quinidine can cause cinchonism (headache, tinnitus), Procainamide can cause drug-induced lupus, and Disopyramide can cause heart failure.
- IB: Lidocaine can cause CNS effects and cardiovascular depression.
- IC: Flecainide can be proarrhythmic, particularly post-MI.
Class II (Beta Blockers)
- Examples: Propranolol, Esmolol, Metoprolol. These drugs reduce heart rate and conduction velocity, which decreases the frequency of arrhythmias.
Class III (K+ Channel Blockers)
- Examples: Amiodarone, Sotalol. These drugs prolong the AP duration and refractoriness, making them useful in treating atrial and ventricular arrhythmias.
- Adverse Effects: Amiodarone has many including pulmonary fibrosis, hepatotoxicity, and thyroid dysfunction.
- Examples: Verapamil, Diltiazem. These drugs slow conduction through the AV node, making them useful in treating supraventricular arrhythmias.

Class V (Miscellaneous)
- Adenosine: Used for terminating paroxysmal supraventricular tachycardia (PSVT).
- Digoxin: Increases vagal tone and decreases conduction through the AV node.
- Mg++: Used in the management of torsades de pointes and digoxin toxicity.
Clinical Implications
- The choice of antiarrhythmic drug depends on the specific type of arrhythmia, the patient's overall health, and potential drug side effects or toxicities.
Normal tissue action potential and changes after drug treatment are pivotal to understanding the effectiveness and risks associated with different classes of antiarrhythmics. Proper titration and monitoring are essential for optimal patient outcomes. Adverse effects can range from arrhythmias to systemic toxicities, necessitating careful selection and use of these medications.