Autonomics of the Pelvis: Detailed Overview
Autonomics of the Pelvis
Sympathetic and Parasympathetic Systems in the Pelvis
Sympathetic System
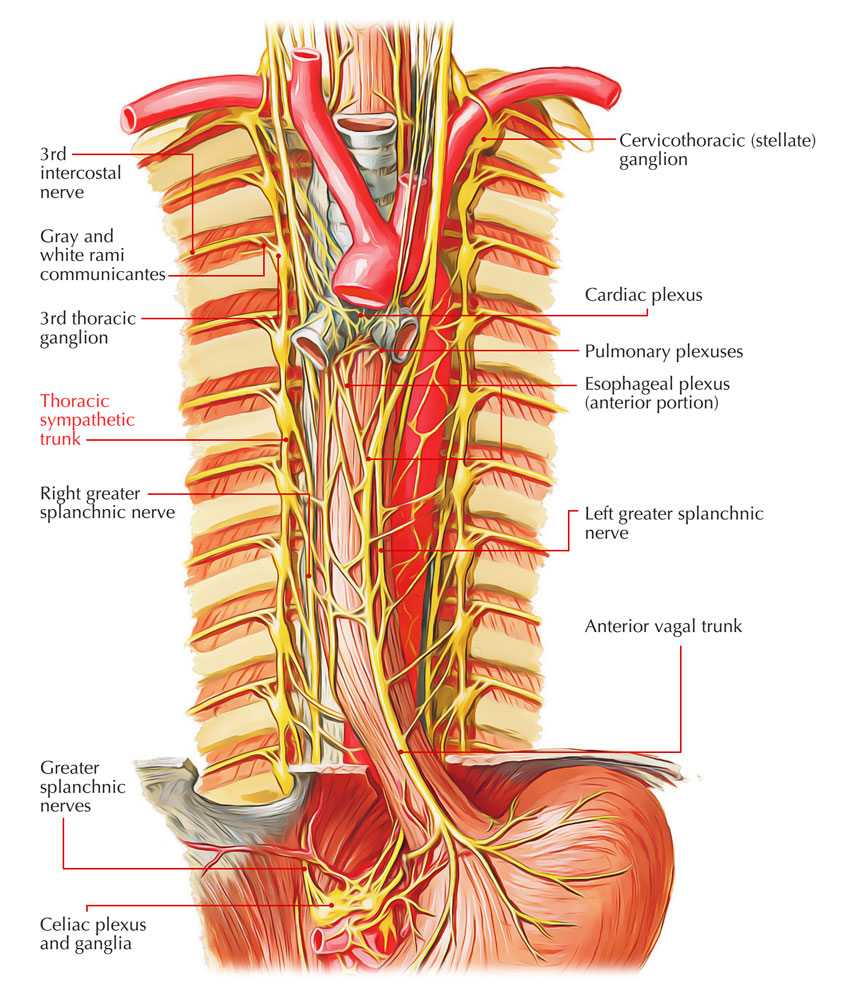
The sympathetic input to the pelvic region primarily originates from the sympathetic trunk and extends into various splanchnic nerves. Here are the main components:
- Sympathetic Chain: The sympathetic trunk runs along the side of the vertebral column and conveys sympathetic nerves to various body parts.
- Gray Rami Communicantes: These are nerve fibers connecting the sympathetic ganglia of the sympathetic trunk to the spinal nerves, allowing postganglionic sympathetic neurons to reach their target organs.
- Sacral Splanchnic Nerves: These nerves arise in the sacral part of the sympathetic trunk and contain postganglionic sympathetic fibers. They help innervate the pelvic organs by connecting to the inferior hypogastric plexus.
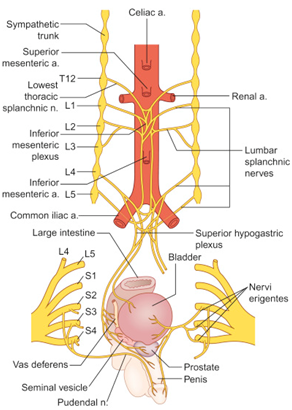
- Lumbar Splanchnic Nerves: These nerves carry both preganglionic and postganglionic sympathetic fibers and connect the lumbar region to the pelvic plexus. Some of these axons synapse in the inferior mesenteric ganglion and then travel through the superior hypogastric plexus (SHP) to the hypogastric nerves (HN) and finally into the pelvic plexus (PP).
Parasympathetic System
The parasympathetic input to the pelvic region is provided by the pelvic splanchnic nerves, which originate directly from the sacral spinal segments S2 to S4.
- Pelvic Splanchnic Nerves: These nerves carry presynaptic parasympathetic fibers from S2 to S4. They enter into the inferior hypogastric plexus and from there innervate the pelvic organs.
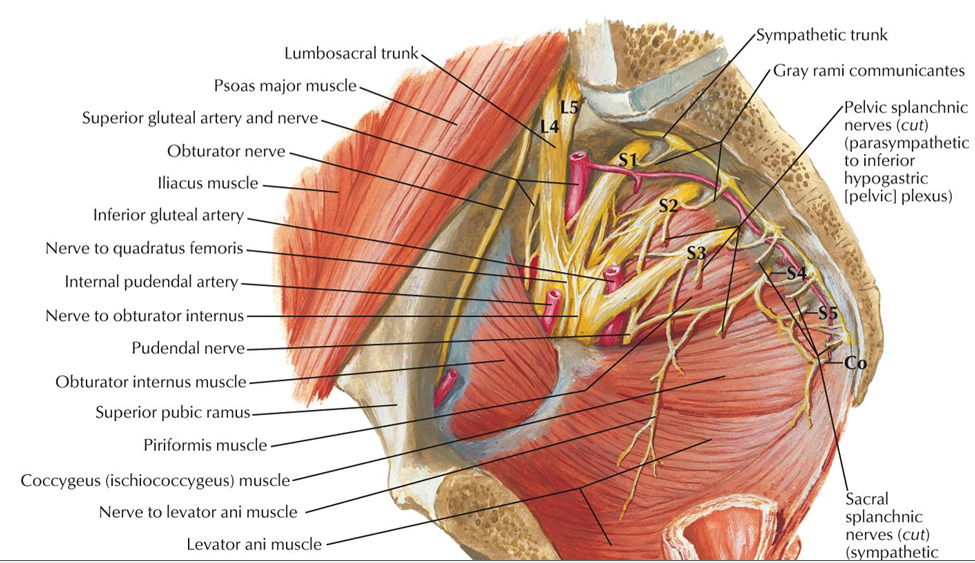
- Inferior Hypogastric Plexus: Also known as the pelvic plexus, it receives contributions from both sympathetic and parasympathetic fibers. This plexus surrounds the pelvic organs and distributes autonomic fibers to them.

Key Plexuses and Nerves
There are several important plexuses and nerves in the pelvic autonomic system:
- Superior Hypogastric Plexus: A plexus that sits on the aorta and receives contributions primarily from lumbar splanchnic nerves. It is a part of the pathway for sympathetic innervation to the pelvis.

- Hypogastric Nerves: These extend from the superior hypogastric plexus and descend into the pelvic region, connecting to the inferior hypogastric plexus.
:background_color(FFFFFF):format(jpeg)/images/article/en/hypogastric-nerve/AtiYThhA42W6YEDxLWwLA_hypogastric_nerve.png)
- Inferior Hypogastric Plexus: A network of autonomic nerves that enwraps the pelvic organs. It contains fibers from both the sympathetic trunk (sacral splanchnic nerves) and parasympathetic fibers (pelvic splanchnic nerves).

- Pudendal Nerve: Although mainly somatic, it has close relationships with autonomic fibers, particularly concerning the control of bladder and rectal functions.
- Visceral Pain Fibers (GVA): They follow the same pathways of autonomic nerves but are responsible for conducting pain and other visceral sensations.

Functional Pathways
Sympathetic Nervous System (SNS):
- Presynaptic sympathetic neurons are located in the spinal cord segments of T1-L2.
- They traverse through the white rami communicantes into the sympathetic trunk.
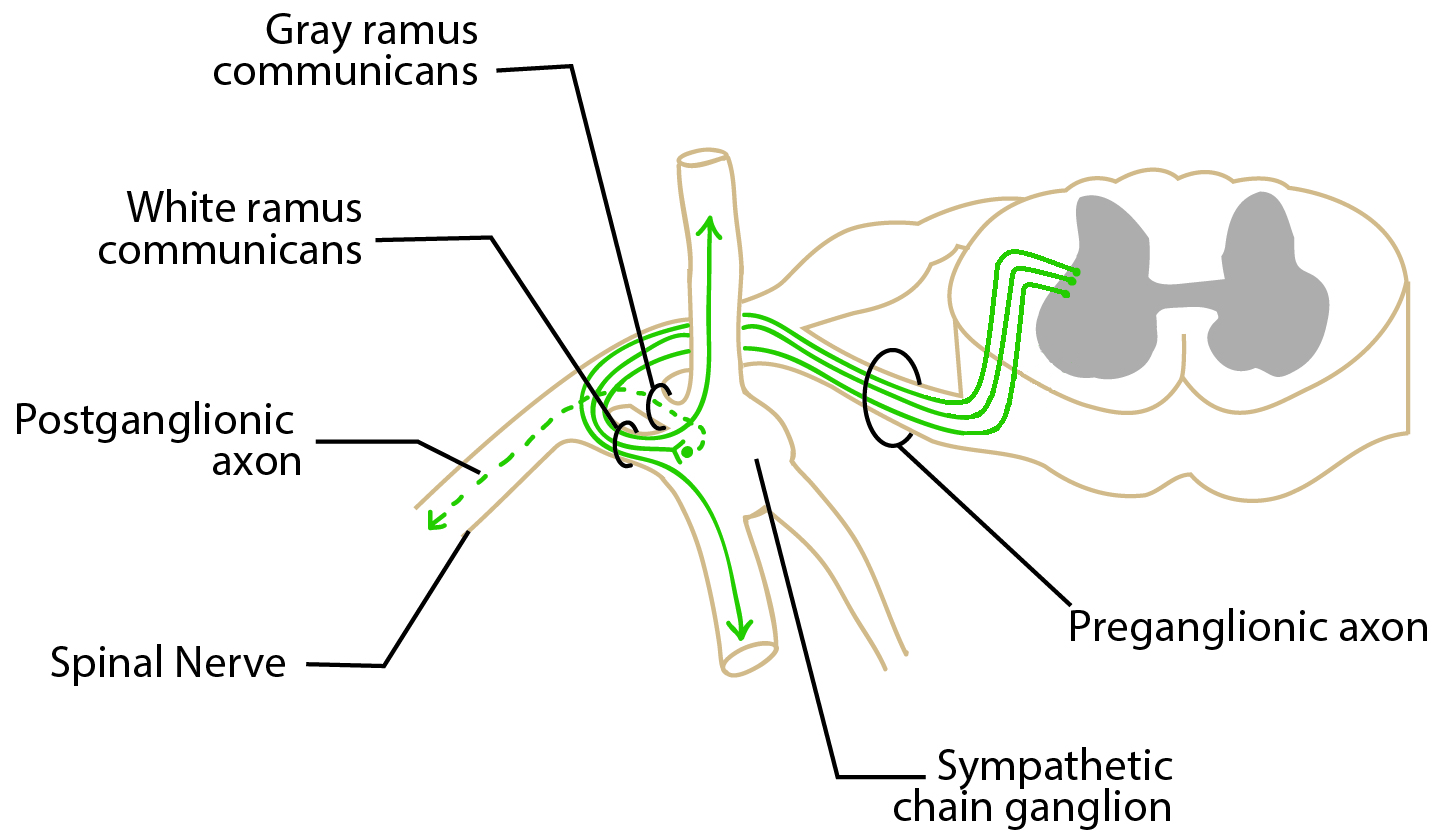
- Synapse are at different levels within the sympathetic trunk or in prevertebral ganglia, such as the inferior mesenteric ganglion.
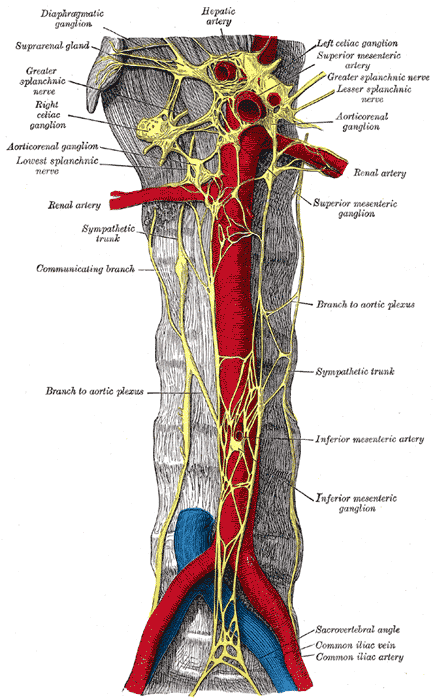
- Extend post-synaptically via gray rami communicantes, targeted nerves, or splanchnic nerves to the intended organs.
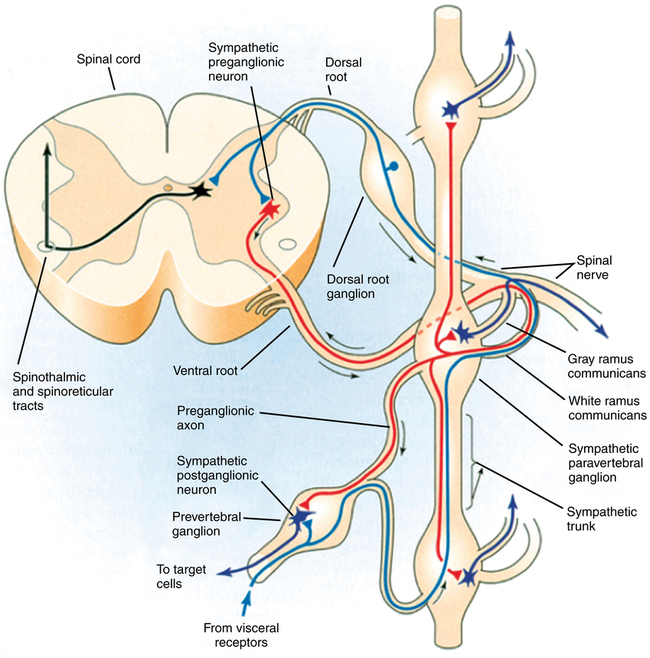
Parasympathetic Nervous System (PSNS):
- Presynaptic parasympathetic neurons are primarily localized in the sacral spinal cord (S2-S4).
- They travel via ventral rami of spinal nerves and establish the pelvic splanchnic nerves.

- Enter inferior hypogastric plexus and branch out to innervate pertinent pelvic structures.
Clinical Relevance: Damage and Dysfunction
- Fracture of the Cribriform Plate: This is a skull structure in the anterior cranial fossa, vulnerable to fracture due to its thinness. Consequences include anosmia (loss of smell) due to damage to olfactory nerve fibers and cerebrospinal fluid (CSF) leakage into the nasal cavity, visible as a clear fluid.
- Impairments in Erectile Function: Damage to the cavernous nerves, which carry parasympathetic fibers crucial for erection, may lead to impotence.
Understanding the autonomics of the pelvis is crucial for diagnosing and treating various functional disorders associated with pelvic organs, including bladder control, sexual function, and rectal disorders.
