Genetic Testing: Definitions, Types, and Applications
Genetic Testing
Objectives
- Define the term genetic testing and its different indications.
- Describe chromosome analysis, microarray analysis, gene sequencing technology, and their utility in diagnosing individuals with suspected conditions and/or at risk for genetic conditions.
- Describe the challenges/limitations of genetic testing, particularly whole exome and genome sequencing, cell-free DNA testing, and direct-to-consumer testing.
- Discuss the differences between diagnostic, carrier, and pre-symptomatic testing.
Genetic Disease
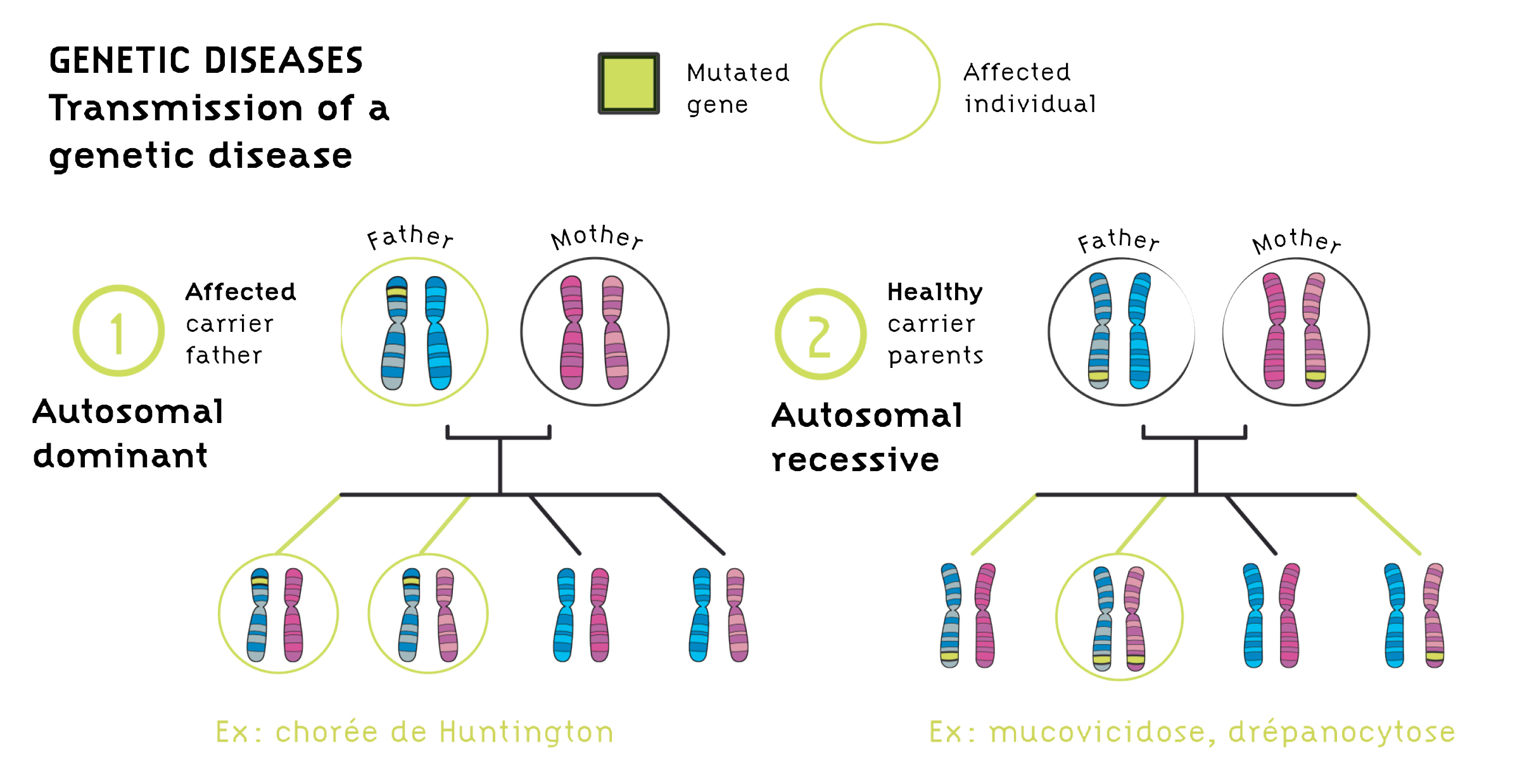
Definition: A genetic disease is a condition caused by a change in the genetic material. Genetic diseases can be classified into several categories: - Single gene disorders (e.g., Achondroplasia) - Chromosome disorders (e.g., Down syndrome) - Epigenetic/Imprinting disorders (e.g., Angelman syndrome) - Multifactorial conditions (e.g., Cleft lip/palate)
Not all genetic diseases are inherited. They can also be sporadic/de novo or acquired.
Genetic Testing: Definition
Genetic testing refers to the use of medical tests that identify changes in chromosomes, genes, or proteins. The results of genetic tests can confirm or rule out a suspected genetic condition or help determine a person’s chance of developing or passing on a genetic disorder.
Purposes of Genetic Testing
- Diagnostic: To identify the cause of a condition.
- Carrier identification
- Newborn screening
- Prognosis
- Pharmacogenetic testing (e.g., psychological, neurological conditions)
- Prenatal testing
- Presymptomatic testing (e.g., Huntington's disease)
- Preimplantation diagnosis
How Genetic Tests Differ From Other Tests
- Some genetic tests assess the risk for future disease.
- Genetic test results often have implications for family members.
- Some family members may prefer not to know the results.
- The best person to test may not necessarily be the patient.
Types of Genetic Testing
Cytogenetics
Karyotype: This involves chromosome analysis to detect abnormalities.
Fluorescence In Situ Hybridization (FISH): Uses labeled chromosome-specific DNA probes to determine if portions of chromosomes are deleted or duplicated.
DNA Microarray Analysis (Comparative Genomic Hybridization - CGH): Measures changes in DNA copy number to detect genomic imbalances.
Diagnostic Genetic Testing
Karyotype Indications
- Birth defects
- Growth and developmental abnormalities
- Family history of chromosome abnormality
- Suspected chromosome abnormality
- Infertility/history of pregnancy loss
- Pregnancy in a female who is of advanced maternal age (>35)
- Stillbirth
- Cancer
Fluorescence In Situ Hybridization (FISH)
Used to determine deletions or duplications in chromosomes by hybridizing labeled probes to chromosomes and visualizing under a microscope.
Microarray (CGH)
Detects pathogenic copy number abnormalities in infants/children with developmental delay, intellectual disability, and/or multiple congenital anomalies. CGH is the recommended first-tier clinical diagnostic test in these evaluations.
CGH Advantages and Disadvantages
- Advantages: Superior for detecting genomic copy number changes. Determines the exact size and location of the abnormality.
- Disadvantages: Cannot detect balanced rearrangements, low-level mosaicism, or single-point mutations. Relatively expensive, and not all copy number changes are clinically significant.
Methylation Testing
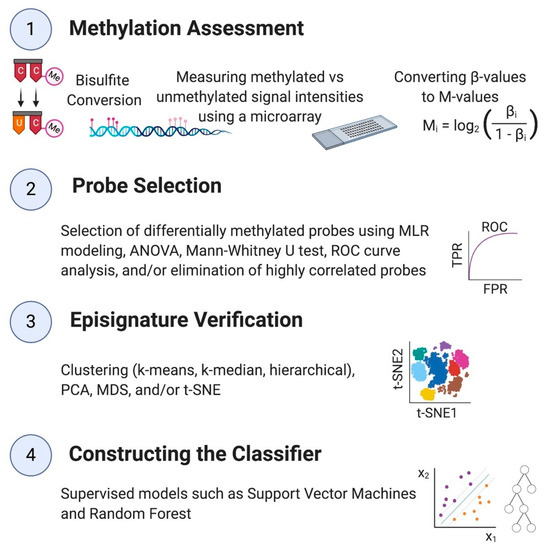
Used to detect conditions like Prader-Willi syndrome and Angelman syndrome by assessing the methylation pattern of specific genomic regions.
Sequencing
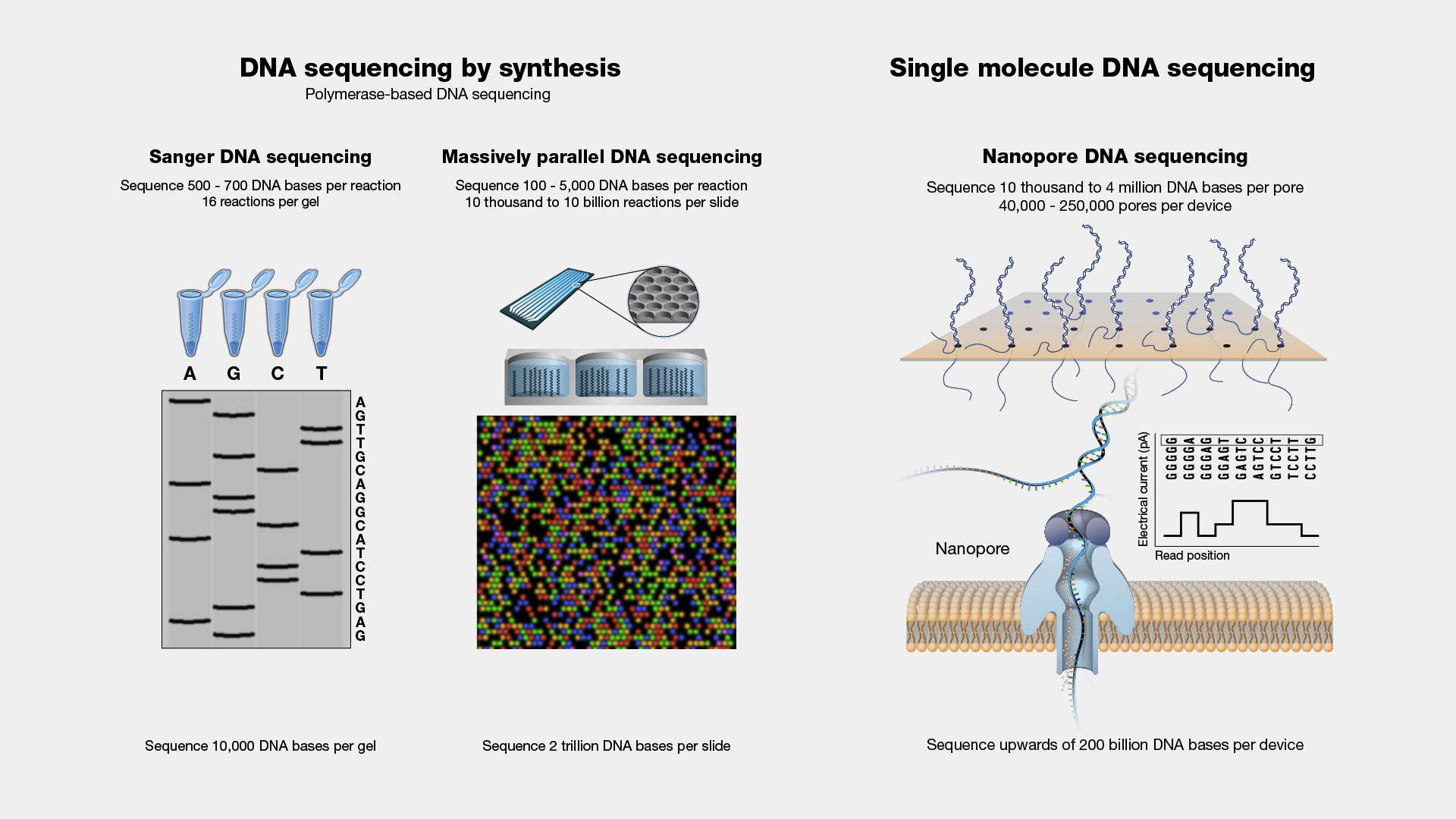
Single Gene Sequencing
- Sanger sequencing is used for high precision but is labor-intensive and expensive.
Next-Generation Sequencing (NGS)
- Panels: Genetic tests that assess multiple genes for specific phenotypes, such as seizures or intellectual disability.
- Whole Exome Sequencing (WES): Focuses on the exons of genes, which contain 85% of known mutations. WES is comprehensive but expensive and may provide unexpected results.
Trinucleotide Repeat Disorders

Examples: Fragile X syndrome, Huntington’s disease. These disorders are characterized by the repetition of nucleotides that affect gene function.
Cell-Free Fetal DNA Testing
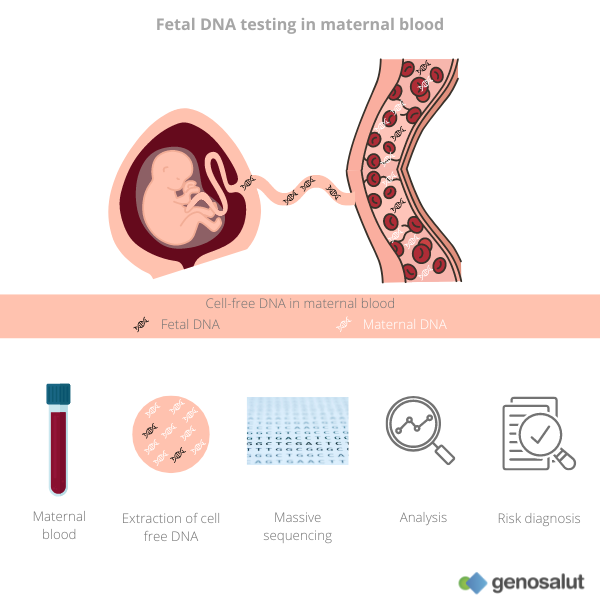
Refers to sampling fetal DNA from maternal blood to perform various genetic tests. This is a screening test with limitations such as false positives and negatives.
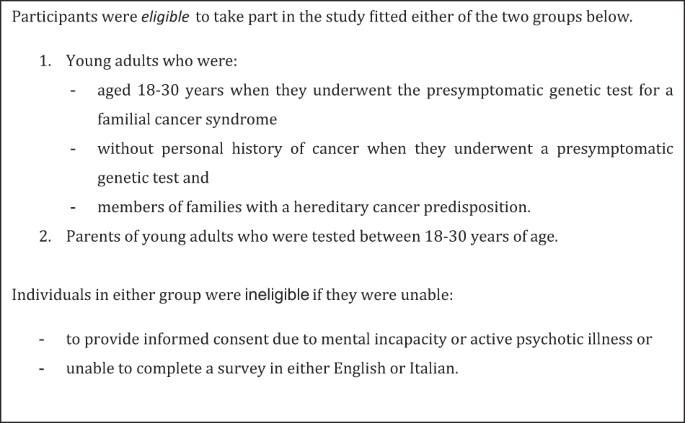
Presymptomatic Genetic Testing
Performed in asymptomatic individuals at risk for disorders they might develop in the future, such as Huntington’s disease and certain cancers. A positive result does not specify when symptoms will appear.
Carrier Testing

Used to identify individuals who carry a genetic change that could be inherited by offspring, often requiring testing of both partners.
Direct to Consumer Testing

Advertised and sold directly to the public, offering information on ancestry, disease risks, drug responses, etc. Concerns include a high false-positive rate, confidentiality issues, and lack of genetic counseling.