Myoglobin and Hemoglobin: Structure, Function, and Clinical Importance
Myoglobin and Hemoglobin
1. Functions of Myoglobin and Hemoglobin
Myoglobin:
- Found in muscle tissue.
- Functions as an oxygen storage molecule, releasing oxygen during intense muscular activity when oxygen levels are low.
- Binds oxygen with high affinity and does not release it easily, which is why it’s efficient in storing oxygen.
Hemoglobin:
- Found in red blood cells.
- Functions to transport oxygen from the lungs to tissues and to carry carbon dioxide back from tissues to the lungs.
- Hemoglobin binds oxygen in the lungs (where oxygen concentration is high) and releases it in tissues (where oxygen concentration is low).
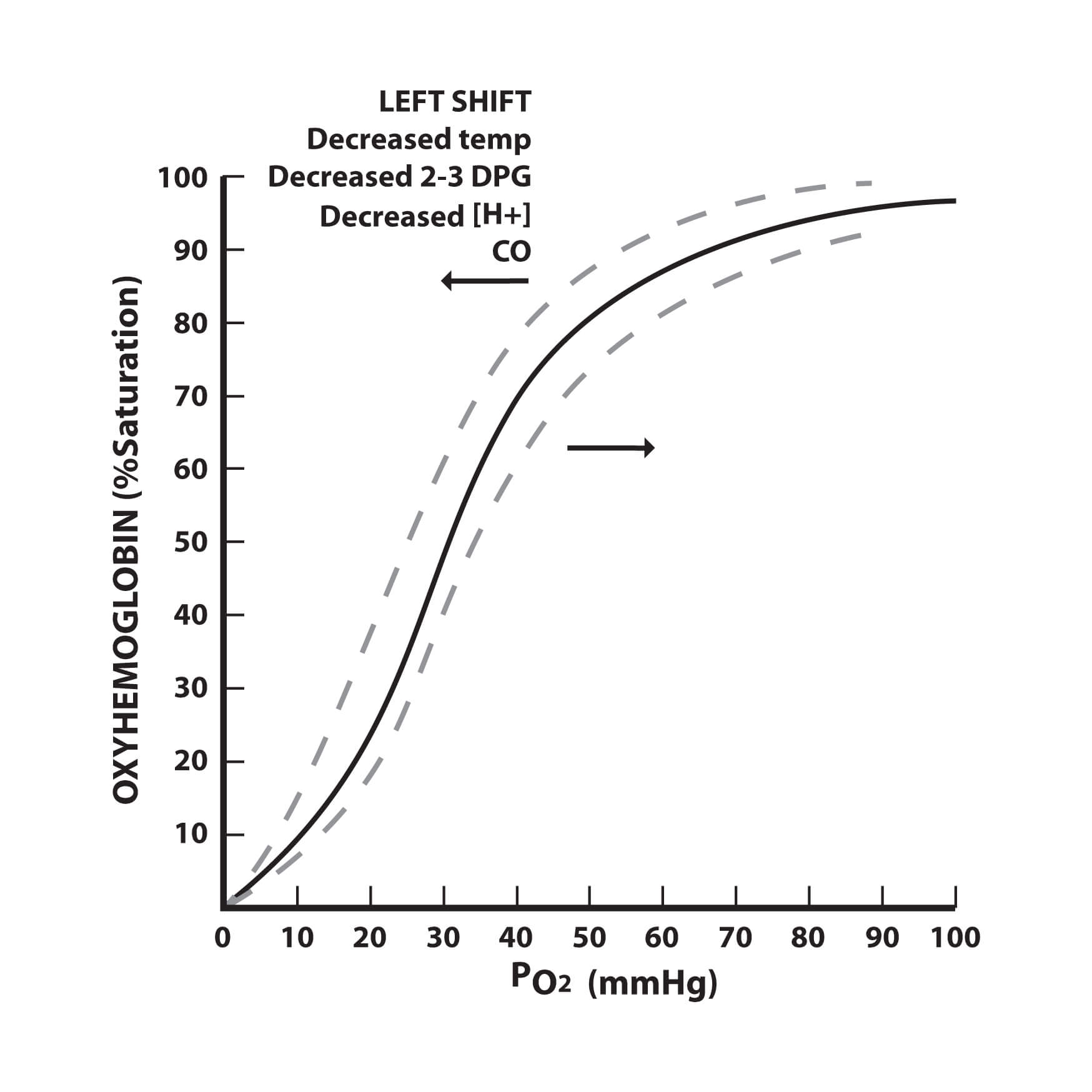
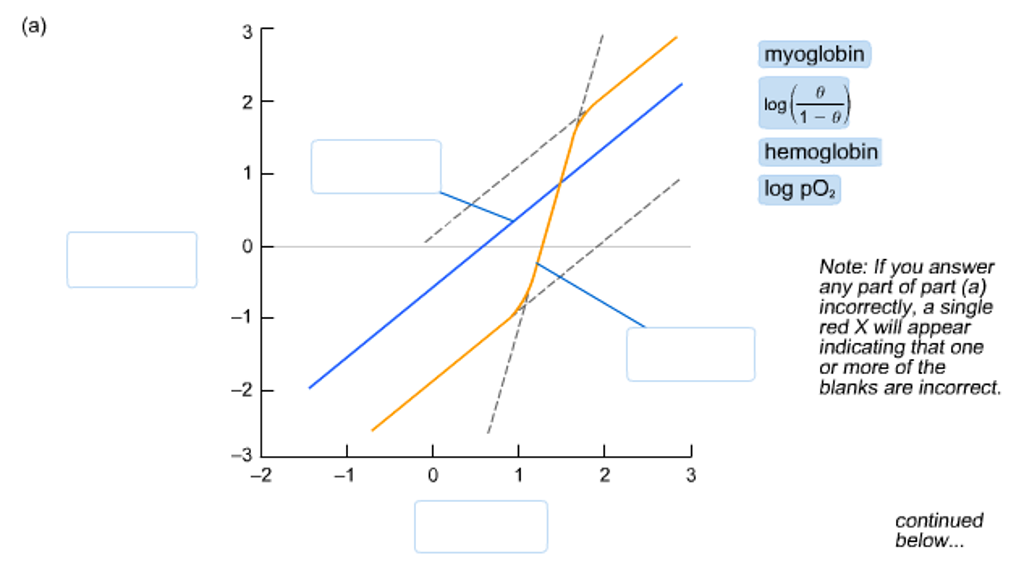
2. Interpreting an Oxygen Saturation Curve
- Oxygen Saturation Curve:
- The curve shows the relationship between the partial pressure of oxygen (pO2) and the percentage of hemoglobin saturated with oxygen.
- Sigmoidal Shape: The curve is sigmoidal due to cooperative binding, where binding of one oxygen molecule increases the affinity of hemoglobin for subsequent oxygen molecules.
- Left Shift: Indicates increased oxygen affinity (hemoglobin holds onto oxygen more tightly).
- Right Shift: Indicates decreased oxygen affinity (hemoglobin releases oxygen more easily).
3. Conditions That Change Oxygen Affinity of Hemoglobin
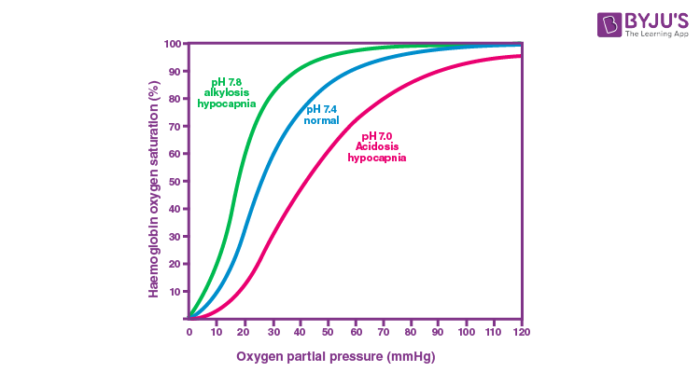
- Bohr Effect:
- Describes how pH and CO2 levels influence hemoglobin’s oxygen-binding affinity.
- pH: Decreased pH (acidic conditions) reduces oxygen affinity (right shift), facilitating oxygen release in tissues where metabolism produces more acid (e.g., lactic acid).
- CO2: Increased CO2 levels reduce oxygen affinity (right shift) because CO2 binds to hemoglobin, stabilizing the deoxygenated form.
- 2,3-Bisphosphoglycerate (2,3-BPG): This molecule binds to hemoglobin and decreases its oxygen affinity, promoting oxygen release in tissues, especially under conditions of low oxygen availability (e.g., high altitude).
4. Structure/Function Relationships in Hemoglobin
T (Tense) and R (Relaxed) States:
- T-State: Hemoglobin is in a low-affinity state for oxygen, prevalent when oxygen levels are low.
- R-State: Hemoglobin is in a high-affinity state, prevalent when oxygen is bound, promoting the binding of additional oxygen molecules.
Allosteric Regulation:
- Hemoglobin's function is regulated allosterically, meaning that the binding of oxygen or other molecules (like CO2, H+, and 2,3-BPG) at one site on the hemoglobin molecule induces conformational changes that affect oxygen binding at other sites.
Mutations:
- Changes in hemoglobin's amino acid sequence can alter its structure, affecting oxygen binding and release.
- For example, the sickle-cell mutation (substitution of valine for glutamic acid at position 6 of the beta chain) causes hemoglobin to polymerize under low oxygen conditions, leading to distorted red blood cells that impair oxygen delivery.
Overview
Oxygen Transport in Multicellular Organisms
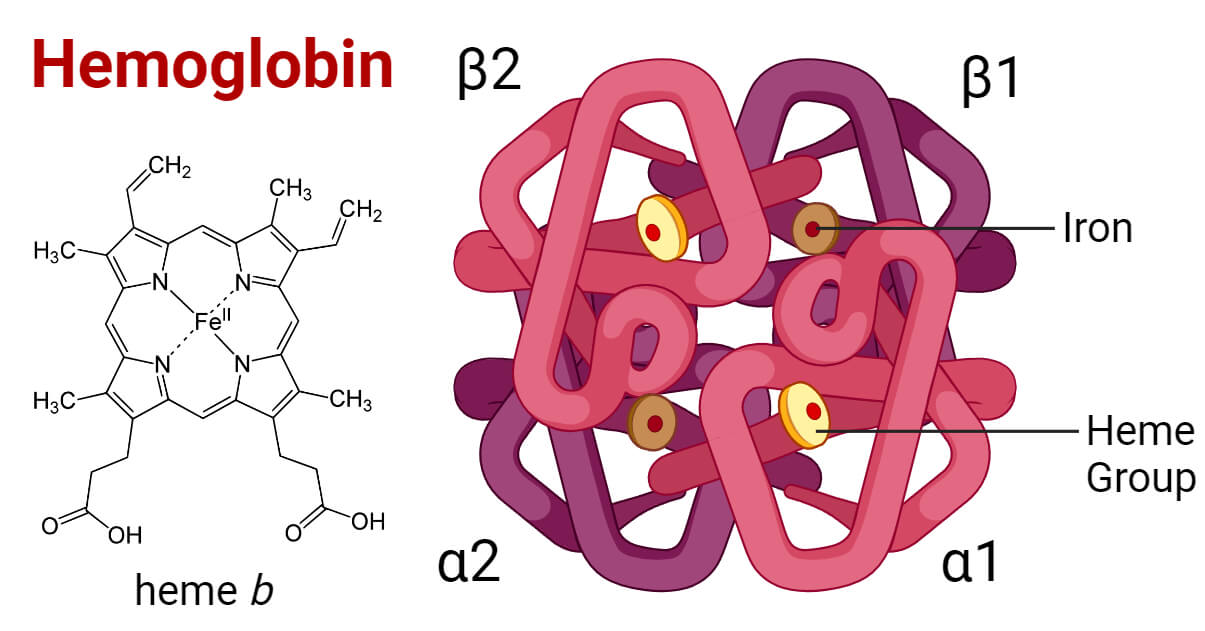
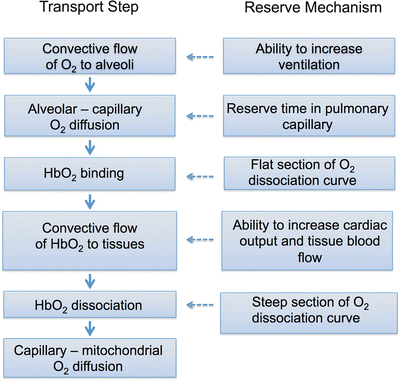
Oxygen transport in multicellular organisms utilizes heme. Oxygen is poorly soluble in aqueous solutions at physiological pH (< 0.0001 M) and cannot be transported effectively to tissues by blood serum. Transition metals, such as iron and copper, readily bind oxygen, but free iron can produce reactive oxygen species that damage biological macromolecules. The heme prosthetic group provides organisms with a means of transporting oxygen to tissues in sufficient quantities to support aerobic metabolism.

Heme Group and Ferrous Iron
Myoglobin and hemoglobin possess heme, a cyclic tetrapyrrole, which coordinates atoms of ferrous iron (Fe2+). Electron-donating pyrrole nitrogen atoms prevent the conversion of Fe2+ to Fe3+, which does not bind oxygen.
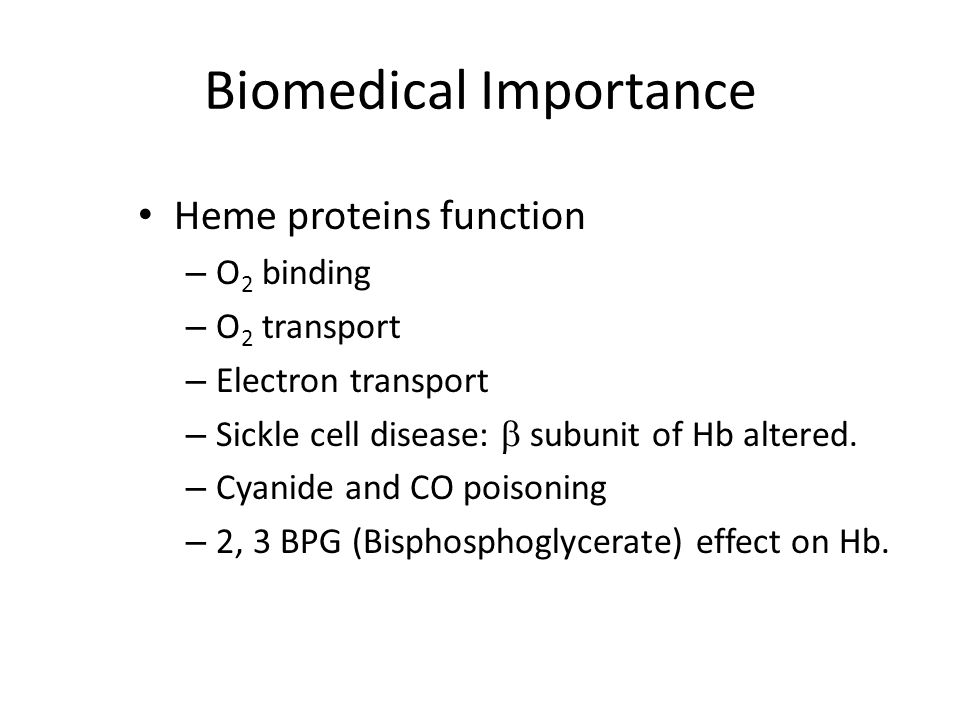
Biomedical Relevance of Heme-Containing Proteins
Heme-containing proteins function in oxygen binding/transport, drug metabolism, and electron transport. Myoglobin and hemoglobin studies have been central to understanding structure-function relationships in globular proteins and the molecular basis of genetic diseases such as sickle cell anemia and thalassemias. Cyanide and carbon monoxide are lethal because they disrupt the physiological functions of cytochrome oxidase, myoglobin, and hemoglobin. Spectroscopic differences between oxygen-bound and deoxygenated heme serve as the basis for functional magnetic resonance imaging (fMRI).
Myoglobin
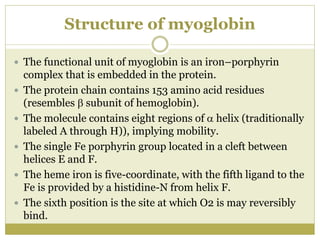
Function and Structure
Myoglobin stores oxygen in muscle tissue and releases it during oxygen deprivation for ATP synthesis in muscle mitochondria. Myoglobin's surface has polar residues, and its interior has mainly non-polar residues. Two histidine residues in the interior function in oxygen binding. Myoglobin is rich in alpha-helical regions, which significantly decrease when heme is removed.

Oxygen Affinity
The affinity of myoglobin for O2 is such that O2 is readily released in oxygen-deprived muscle tissue when partial pressure of O2 (pO2) is 5-10 mm Hg.
Hemoglobin

Transport Functions
Hemoglobins of vertebrate erythrocytes perform two major transport functions: 1. Transport of O2 from the respiratory organ to peripheral tissues 2. Transport of CO2 and protons from peripheral tissue to the respiratory organ for subsequent release
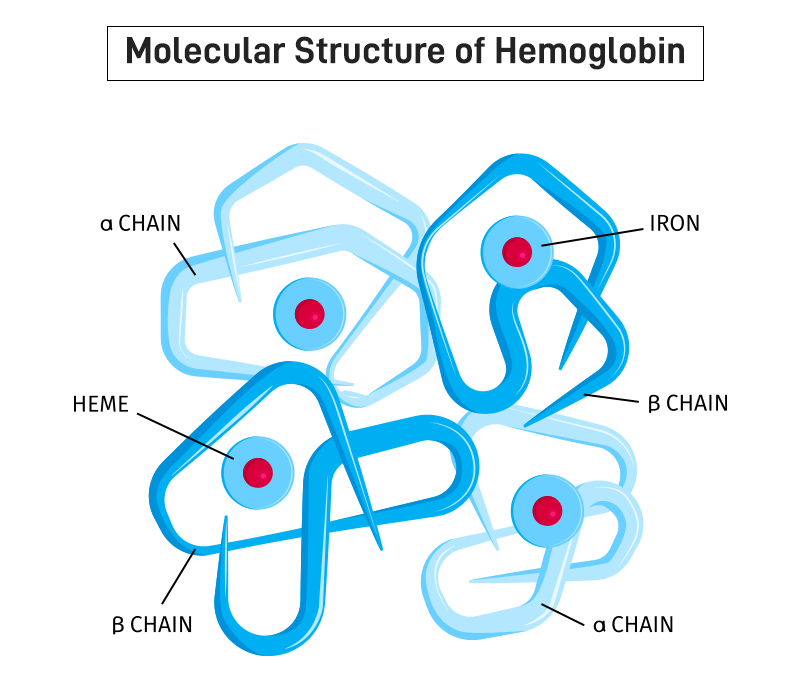
Structural Composition
Hemoglobins are tetrameric proteins composed of pairs of two different polypeptides (α, β, γ, δ). Human hemoglobin A (HbA) consists of α2β2 subunits. Hemoglobin variants include fetal hemoglobin (HbF, α2γ2), sickle cell hemoglobin (HbS, α2S2), and minor adult form hemoglobin (HbA2, α2δ2).
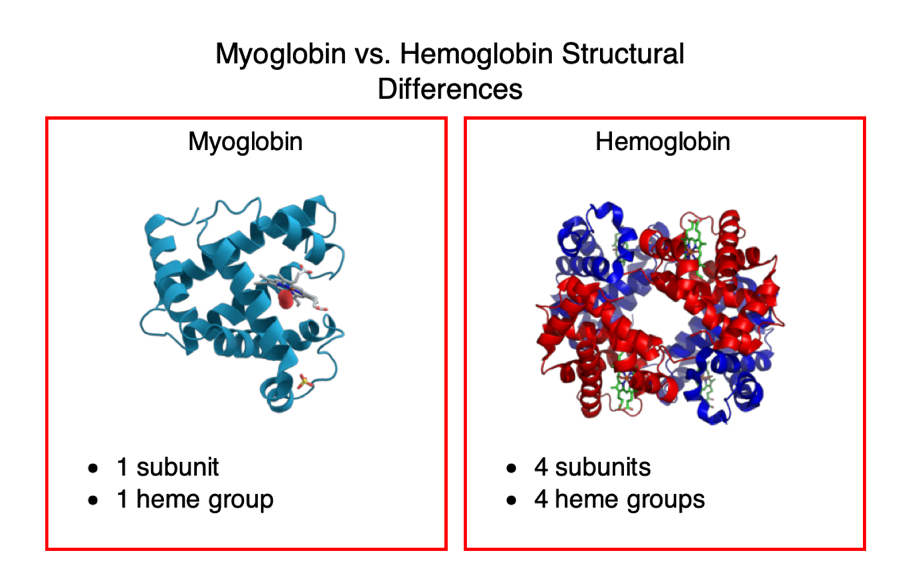
Myoglobin vs. Hemoglobin
While myoglobin and hemoglobin subunits have nearly identical secondary and tertiary structures, myoglobin is monomeric, and hemoglobin is a tetramer with four subunit interactions. Hemoglobin's binding of oxygen shows cooperative kinetics due to allosteric effects.
Conformational Changes and Oxygen Affinity
Hemoglobin undergoes a transition from a low affinity (T) state to a high affinity (R) state as more oxygen molecules are bound. This cooperative binding mechanism increases the O2 that hemoglobin can transport.

Bohr Effect
The Bohr effect describes how pH, CO2, and 2,3-bisphosphoglycerate (BPG) influence hemoglobin's oxygen affinity. Increased acidity (lower pH) promotes oxygen unloading in tissues. BPG stabilizes the T conformation, reducing oxygen affinity and facilitating oxygen release in capillaries.

CO2 Transport
Hemoglobin also transports CO2 directly by forming carbamino-hemoglobin at peripheral tissues, stabilizing the T-form, and contributing to the Bohr effect. Additionally, CO2 is transported as bicarbonate in plasma through isohydric transport.
:max_bytes(150000):strip_icc()/VWH-JessicaOlah-CommonSymptomsofCarbonMonoxidePoisoning-Standard-460087eaa2ad4058af35e4606caabe07.jpg)
Carbon Monoxide Poisoning
CO binds to hemoglobin 230 times more tightly than oxygen, leading to impaired oxygen release in tissues. Symptoms range from headache to death depending on CO exposure, and poisoning is treated with 100% oxygen therapy.
Summary
Understanding the molecular structure and function of myoglobin and hemoglobin is critical for interpreting their roles in oxygen transport and storage, as well as their clinical implications in conditions like anemia, sickle cell disease, and carbon monoxide poisoning.