The Cervical and Cranial Nerves
The Cervical and Cranial Nerves
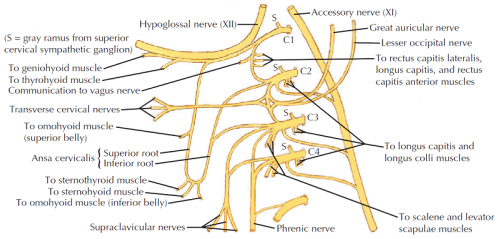
Cervical Plexus Overview
The cervical plexus is formed by the ventral rami of the spinal nerves C1-C4. Beyond the roots, there are mixed nerves comprising both afferent (sensory) and efferent (motor) components. Key nerves in the cervical plexus include CN XII, CN XI, and the phrenic nerve.
Cutaneous Branches (Superficial)
- Lesser occipital nerve (C2): Innervates the skin of the neck and scalp posterior and superior to the auricle.
- Great auricular nerve (C2, C3): Supplies the skin over the parotid gland, mastoid process, and both surfaces of the auricle.
- Transverse cervical nerve (C2, C3): Innervates the skin of the anterior triangle of the neck.
- Supraclavicular nerves (medial, intermediate, lateral) (C3, C4): Innervate the skin over the shoulder.
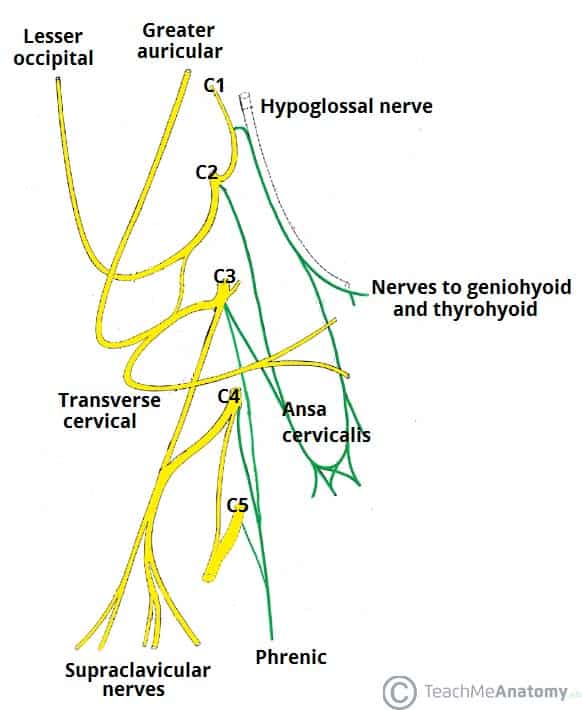
Motor Branches (Deep)
- Ansa cervicalis: Contains motor fibers that innervate the infrahyoid muscles.
- Phrenic nerve: Innervates the diaphragm, playing a crucial role in respiration.
- Branches to the scalene muscles: Provide motor innervation to the scalene muscles including the anterior, middle, and posterior scalene.
Cranial Nerves Overview
Cranial nerves have various functional components and can carry afferent (sensory), efferent (motor), or both types of axons. Here's a detailed breakdown:
Functional Components of Cranial Nerves
Afferent (Sensory)
- General Somatic Afferents (GSA): Nerve fibers that carry sensory information from the skin.
- General Visceral Afferents (GVA): Nerve fibers that carry pain and stretch sensations from organs.
- Special Afferents (SA): Nerve fibers that convey information about senses such as smell, taste, sight, hearing, and balance.
Efferent (Motor)
- General Somatic Efferents (GSE): Nerve fibers that convey motor information to skeletal muscles.
- Special Visceral Efferent/Branchial Efferent (SVE/BE): Nerve fibers that innervate structures derived from pharyngeal arches.
- General Visceral Efferents (GVE): Nerve fibers that carry parasympathetic information to smooth muscle, glands, and cardiac muscle.

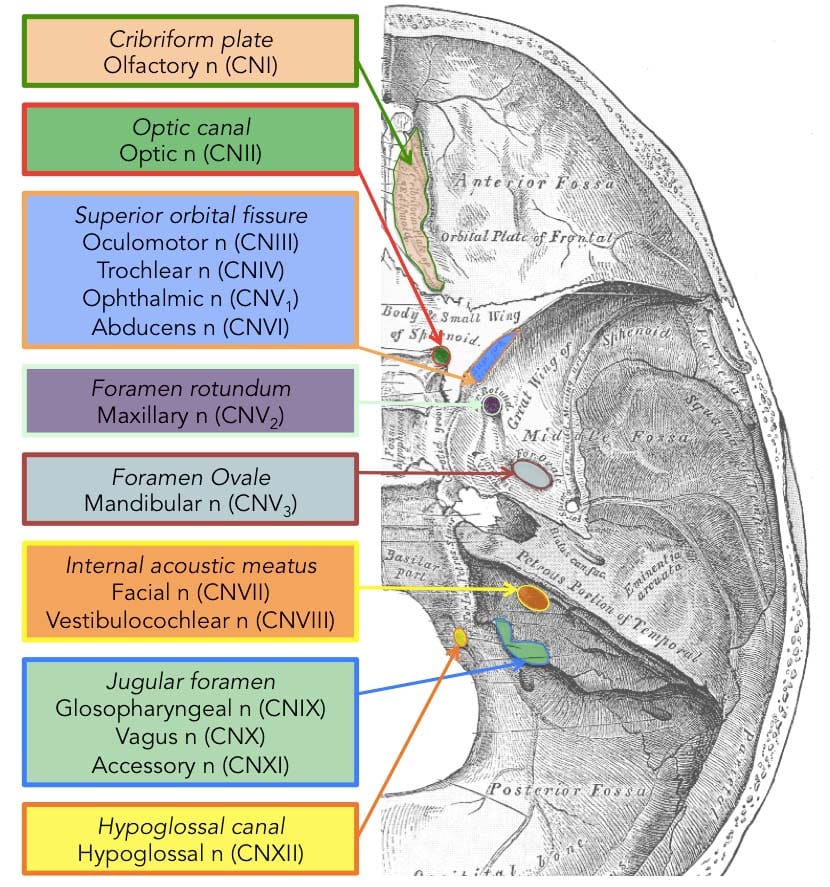
Segmentation and Exit of Cranial Nerves
Foramina and Cranial Nerves
- Olfactory (I): Cribriform Plate
- Optic (II): Optic Canal
- Oculomotor (III): Superior Orbital Fissure
- Trochlear (IV): Superior Orbital Fissure
- Trigeminal (V): V1 (Superior Orbital Fissure), V2 (Foramen Rotundum), V3 (Foramen Ovale)
- Abducens (VI): Superior Orbital Fissure
- Facial (VII): Internal Acoustic Meatus
- Vestibulocochlear (VIII): Internal Acoustic Meatus
- Glossopharyngeal (IX): Jugular Foramen
- Vagus (X): Jugular Foramen
- Spinal Accessory (XI): Jugular Foramen
- Hypoglossal (XII): Hypoglossal Canal
Organization of Cranial Nerves by Modality
- Sensory Only: I, II, VIII
- Motor Only: III, IV, VI, XI, XII
- Mixed Sensory and Motor: V, VII, IX, X
Autonomics of the Head and Neck
Sympathetic Pathway
- Presynaptic sympathetic fibers from T1-T4 spinal segments ascend to the cervical sympathetic trunk.
- Postsynaptic sympathetic fibers follow the internal carotid artery into the head as the internal carotid nerve.
Horner Syndrome
Damage to the sympathetic pathways can result in Horner syndrome, characterized by:
- Constricted pupil (miosis)
- Mild drooping of the eyelid (ptosis)
- Lack of sweating on one side of the face (anhydrosis)
- Flushed complexion on one side of the face (vasodilation)
Causes of Horner Syndrome
- Pancoast tumor in the apex of the lung
- Accidental or iatrogenic injury to the sympathetic chain
- Internal carotid artery dissection
- Cavernous sinus thrombosis or internal carotid artery aneurysm

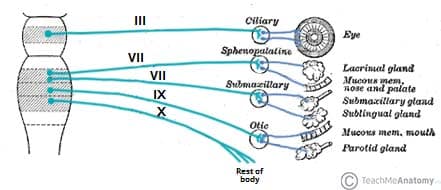
Parasympathetic Pathway
- Preganglionic neurons originate from specific nuclei in the brain and exit with cranial nerves III, VII, IX, and X.
- Postganglionic neurons are located in one of the four named parasympathetic ganglia in the head: Ciliary, Pterygopalatine, Submandibular, and Otic.
Functions of Parasympathetic Ganglia
- Ciliary Ganglion (CN III): Innervates sphincter pupillae and ciliary muscles, affecting pupil dilation and accommodation.
- Dysfunction results in dilated pupils and loss of accommodation.
- Pterygopalatine Ganglion (CN VII): Innervates the lacrimal gland and other minor glands in the palate and sinus regions.
- Dysfunction results in dryness of the eyes.
- Submandibular Ganglion (CN VII): Innervates submandibular and sublingual glands.
- Dysfunction results in dryness of the mouth.
- Otic Ganglion (CN IX): Innervates the parotid gland.
- Dysfunction results in decreased secretion from the parotid gland.
Important Notes
- Cranial nerves III, VII, IX, and X carry presynaptic parasympathetic fibers.
- The vagus nerve (CN X) provides parasympathetic innervation up to the end of the midgut and synapses within the target organs, unlike the other cranial nerves that synapse in named ganglia.
- Summary of the four parasympathetic ganglia:
- Ciliary Ganglion: Targets sphincter pupillae and ciliary muscles (CN III)
- Pterygopalatine Ganglion: Targets lacrimal gland and minor palatal glands (CN VII)
- Submandibular Ganglion: Targets submandibular and sublingual glands (CN VII)
- Otic Ganglion: Targets parotid gland (CN IX)